
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
- Efficacy and Safety of IDegAsp in a Real-World Korean Population with Type 2 Diabetes Mellitus
- Shinae Kang, Yu-Bae Ahn, Tae Keun Oh, Won-Young Lee, Sung Wan Chun, Boram Bae, Amine Dahaoui, Jin Sook Jeong, Sungeun Jung, Hak Chul Jang
- Received August 24, 2023 Accepted November 22, 2023 Published online February 27, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0297 [Epub ahead of print]

- 649 View
- 42 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the real-world efficacy and safety of insulin degludec/insulin aspart (IDegAsp) in Korean adults with type 2 diabetes mellitus (T2DM), whose insulin treatment was switched to IDegAsp.
Methods
This was a multicenter, retrospective, observational study comprising two 26-week treatment periods, before and after switching to IDegAsp, respectively. Korean adults with uncontrolled T2DM treated with basal or premix insulin (±oral antidiabetic drugs) were enrolled. The primary objective was to compare the degree of glycosylated hemoglobin (HbA1c) change in each 26-week observation period. The analyses included changes in HbA1c, fasting plasma glucose (FPG), body weight, proportion of participants achieving HbA1c <7.0%, hypoglycemic events, and total daily insulin dose (ClinicalTrials.gov, number NCT04656106).
Results
In total, 196 adults (mean age, 65.95 years; mean T2DM duration, 18.99 years) were analyzed. The change in both HbA1c and FPG were significantly different between the pre-switching and the post-switching period (0.28% vs. –0.51%, P<0.001; 5.21 mg/dL vs. –23.10 mg/dL, P=0.005), respectively. After switching, the rate of achieving HbA1c <7.0% was significantly improved (5.10% at baseline vs. 11.22% with IDegAsp, P=0.012). No significant differences (before vs. after switching) were observed in body weight change, and total daily insulin dose. The rates of overall and severe hypoglycemia were similar in the two periods.
Conclusion
In real-world clinical practice in Korea, the change of insulin regimen to IDegAsp was associated with an improvement in glycemic control without increase of hypoglycemia, supporting the use of IDegAsp for patients with T2DM uncontrolled with basal or premix insulin.
- Basic Research
- Hypoxia Increases β-Cell Death by Activating Pancreatic Stellate Cells within the Islet
- Jong Jin Kim, Esder Lee, Gyeong Ryul Ryu, Seung-Hyun Ko, Yu-Bae Ahn, Ki-Ho Song
- Diabetes Metab J. 2020;44(6):919-927. Published online May 11, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0181
- 5,938 View
- 146 Download
- 15 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
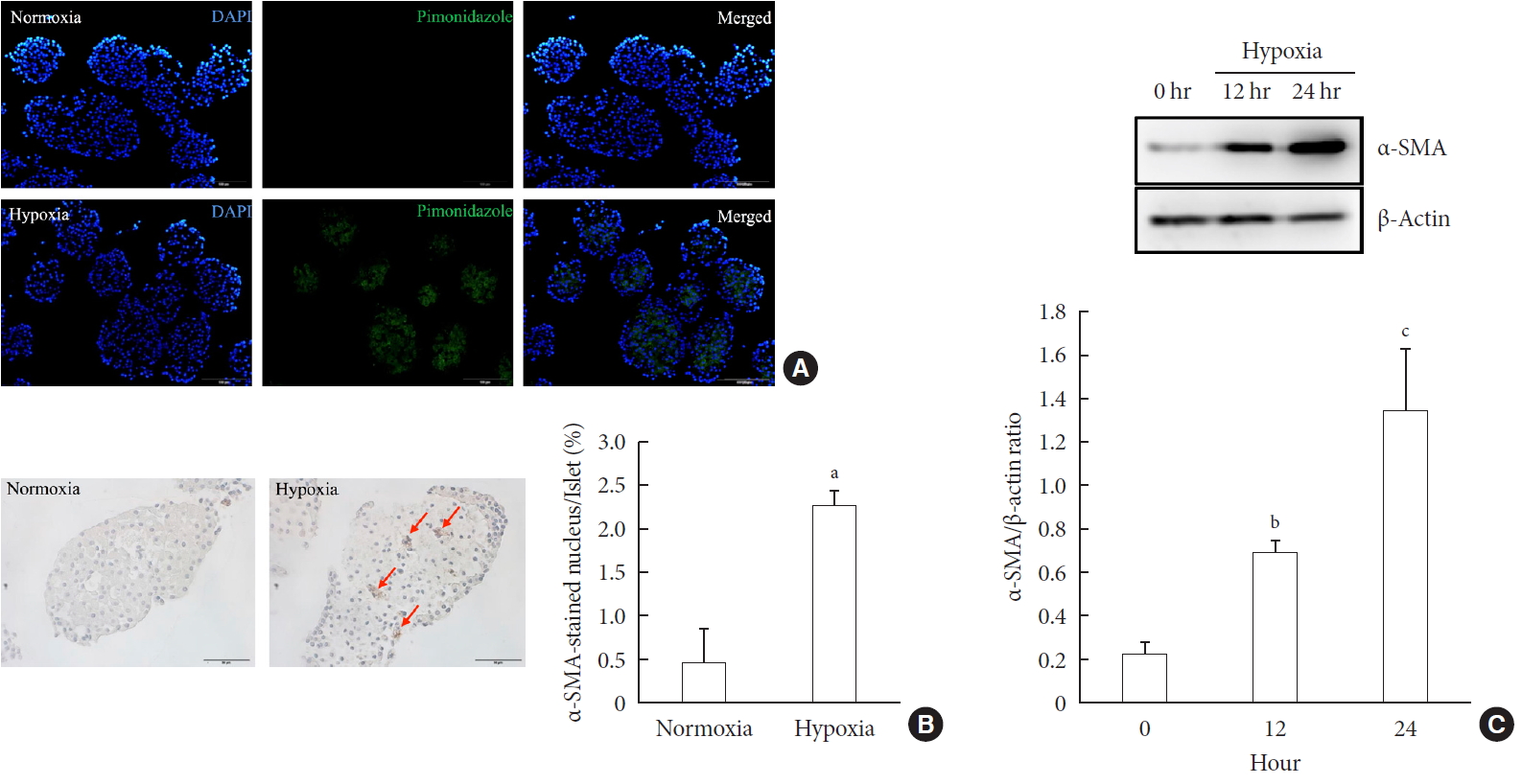
ePub Background Hypoxia can occur in pancreatic islets in type 2 diabetes mellitus. Pancreatic stellate cells (PSCs) are activated during hypoxia. Here we aimed to investigate whether PSCs within the islet are also activated in hypoxia, causing β-cell injury.
Methods Islet and primary PSCs were isolated from Sprague Dawley rats, and cultured in normoxia (21% O2) or hypoxia (1% O2). The expression of α-smooth muscle actin (α-SMA), as measured by immunostaining and Western blotting, was used as a marker of PSC activation. Conditioned media (hypoxia-CM) were obtained from PSCs cultured in hypoxia.
Results Islets and PSCs cultured in hypoxia exhibited higher expressions of α-SMA than did those cultured in normoxia. Hypoxia increased the production of reactive oxygen species. The addition of N-acetyl-L-cysteine, an antioxidant, attenuated the hypoxia-induced PSC activation in islets and PSCs. Islets cultured in hypoxia-CM showed a decrease in cell viability and an increase in apoptosis.
Conclusion PSCs within the islet are activated in hypoxia through oxidative stress and promote islet cell death, suggesting that hypoxia-induced PSC activation may contribute to β-cell loss in type 2 diabetes mellitus.
-
Citations
Citations to this article as recorded by- Effects of hypoxia in the diabetic corneal stroma microenvironment
Purnima Sharma, Jian-Xing Ma, Dimitrios Karamichos
Experimental Eye Research.2024; 240: 109790. CrossRef - Visualizing hypoxic modulation of beta cell secretions via a sensor augmented oxygen gradient
Kai Duan, Mengyang Zhou, Yong Wang, Jose Oberholzer, Joe F. Lo
Microsystems & Nanoengineering.2023;[Epub] CrossRef - Pancreatic stellate cells promote pancreatic β-cell death through exosomal microRNA transfer in hypoxia
Esder Lee, Gyeong Ryul Ryu, Seung-Hyun Ko, Yu-Bae Ahn, Ki-Ho Song
Molecular and Cellular Endocrinology.2023; 572: 111947. CrossRef - Pancreatic stellate cells in pancreatic cancer: as potential targets for future therapy
Zhengfeng Wang, Ru He, Shi Dong, Wence Zhou
Frontiers in Oncology.2023;[Epub] CrossRef - Recent advances in the development of bioartificial pancreas using 3D bioprinting for the treatment of type 1 diabetes: a review
Anushikha Ghosh, Arka Sanyal, Abhik Mallick
Exploration of Medicine.2023; : 886. CrossRef - Pancreas and islet morphology in cystic fibrosis: clues to the etiology of cystic fibrosis-related diabetes
Sarah S. Malik, Diksha Padmanabhan, Rebecca L. Hull-Meichle
Frontiers in Endocrinology.2023;[Epub] CrossRef - Diabetic mellitus, vascular calcification and hypoxia: A complex and neglected tripartite relationship
Xue-Jiao Sun, Nai-Feng Liu
Cellular Signalling.2022; 91: 110219. CrossRef - HIF-1 and NRF2; Key Molecules for Malignant Phenotypes of Pancreatic Cancer
Shin Hamada, Ryotaro Matsumoto, Atsushi Masamune
Cancers.2022; 14(2): 411. CrossRef - Pancreatic Stellate Cells and Metabolic Alteration: Physiology and Pathophysiology
Shin Hamada, Ryotaro Matsumoto, Atsushi Masamune
Frontiers in Physiology.2022;[Epub] CrossRef - Exosomal miR-140–3p and miR-143–3p from TGF-β1-treated pancreatic stellate cells target BCL2 mRNA to increase β-cell apoptosis
Xiangyun Zhu, Dechen Liu, Guoqing Li, Mengmeng Zhi, Ji Sun, Liang Qi, Jingbo Li, Stephen J. Pandol, Ling Li
Molecular and Cellular Endocrinology.2022; 551: 111653. CrossRef - Mitochondria oxidative stress mediated nicotine-promoted activation of pancreatic stellate cells by regulating mitochondrial dynamics
Yue Yuan, Zhiren Li, Miaomiao Li, Tong Jin, Xiaoyun Zhang, Xinjuan Liu, Jianyu Hao
Toxicology in Vitro.2022; 84: 105436. CrossRef - Antioxidant Mitoquinone Alleviates Chronic Pancreatitis via Anti-Fibrotic and Antioxidant Effects
Miaomiao Li, Yue Yuan, Xue Han, Xinjuan Liu, Weizhen Zhang, Jianyu Hao
Journal of Inflammation Research.2022; Volume 15: 4409. CrossRef - Diabetic Ferroptosis and Pancreatic Cancer: Foe or Friend?
Le Li, Xing-jia Yu, Lei Gao, Long Cheng, Bei Sun, Gang Wang
Antioxidants & Redox Signaling.2022; 37(16-18): 1206. CrossRef - Melatonin Induces Apoptosis and Modulates Cyclin Expression and MAPK Phosphorylation in Pancreatic Stellate Cells Subjected to Hypoxia
Matias Estaras, Manuel R. Gonzalez-Portillo, Miguel Fernandez-Bermejo, Jose M. Mateos, Daniel Vara, Gerardo Blanco-Fernandez, Diego Lopez-Guerra, Vicente Roncero, Gines M. Salido, Antonio González
International Journal of Molecular Sciences.2021; 22(11): 5555. CrossRef - Integrated pancreatic microcirculatory profiles of streptozotocin‐induced and insulin‐administrated type 1 diabetes mellitus
Yuan Li, Bingwei Li, Bing Wang, Mingming Liu, Xiaoyan Zhang, Ailing Li, Jian Zhang, Honggang Zhang, Ruijuan Xiu
Microcirculation.2021;[Epub] CrossRef - Pancreatic stellate cells - rising stars in pancreatic pathologies
P Hrabák, M Kalousová, T Krechler, T Zima
Physiological Research.2021; (S4): S597. CrossRef
- Effects of hypoxia in the diabetic corneal stroma microenvironment
- Clinical Diabetes & Therapeutics
- Acarbose Add-on Therapy in Patients with Type 2 Diabetes Mellitus with Metformin and Sitagliptin Failure: A Multicenter, Randomized, Double-Blind, Placebo-Controlled Study
- Hae Kyung Yang, Seung-Hwan Lee, Juyoung Shin, Yoon-Hee Choi, Yu-Bae Ahn, Byung-Wan Lee, Eun Jung Rhee, Kyung Wan Min, Kun-Ho Yoon
- Diabetes Metab J. 2019;43(3):287-301. Published online December 20, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0054
- 5,883 View
- 104 Download
- 14 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We evaluated the efficacy and safety of acarbose add-on therapy in Korean patients with type 2 diabetes mellitus (T2DM) who are inadequately controlled with metformin and sitagliptin.
Methods A total of 165 subjects were randomized to metformin and sitagliptin (Met+Sita,
n =65), metformin, sitagliptin, and acarbose (Met+Sita+Acarb,n =66) and sitagliptin and acarbose (Sita+Acarb, exploratory assessment,n =34) therapy in five institutions in Korea. After 16 weeks of acarbose add-on or metformin-switch therapy, a triple combination therapy was maintained from week 16 to 24.Results The add-on of acarbose (Met+Sita+Acarb group) demonstrated a 0.44%±0.08% (
P <0.001 vs. baseline) decrease in glycosylated hemoglobin (HbA1c) at week 16, while changes in HbA1c were insignificant in the Met+Sita group (−0.09%±0.10%,P =0.113). After 8 weeks of triple combination therapy, HbA1c levels were comparable between Met+Sita and Met+Sita+Acarb group (7.66%±0.13% vs. 7.47%±0.12%,P =0.321). Acarbose add-on therapy demonstrated suppressed glucagon secretion (area under the curve of glucagon, 4,726.17±415.80 ng·min/L vs. 3,314.38±191.63 ng·min/L,P =0.004) in the absence of excess insulin secretion during the meal tolerance tests at week 16 versus baseline. The incidence of adverse or serious adverse events was similar between two groups.Conclusion In conclusion, a 16-week acarbose add-on therapy to metformin and sitagliptin, effectively lowered HbA1c without significant adverse events. Acarbose might be a good choice as a third-line therapy in addition to metformin and sitagliptin in Korean subjects with T2DM who have predominant postprandial hyperglycemia and a high carbohydrate intake.
-
Citations
Citations to this article as recorded by- The effect of acarbose on inflammatory cytokines and adipokines in adults: a systematic review and meta-analysis of randomized clinical trials
Ali Mohammadian, Sahand Tehrani Fateh, Mahlagha Nikbaf-Shandiz, Fatemeh Gholami, Niloufar Rasaei, Hossein Bahari, Samira Rastgoo, Reza Bagheri, Farideh Shiraseb, Omid Asbaghi
Inflammopharmacology.2024; 32(1): 355. CrossRef - An Update on Dipeptidyl Peptidase-IV Inhibiting Peptides
Sachithanantham Annapoorani Sivaraman, Varatharajan Sabareesh
Current Protein & Peptide Science.2024; 25(4): 267. CrossRef - Deciphering Molecular Aspects of Potential α-Glucosidase Inhibitors within Aspergillus terreus: A Computational Odyssey of Molecular Docking-Coupled Dynamics Simulations and Pharmacokinetic Profiling
Sameh S. Elhady, Noha M. Alshobaki, Mahmoud A. Elfaky, Abdulrahman E. Koshak, Majed Alharbi, Reda F. A. Abdelhameed, Khaled M. Darwish
Metabolites.2023; 13(8): 942. CrossRef - Change of metformin concentrations in the liver as a pharmacological target site of metformin after long-term combined treatment with ginseng berry extract
Choong Whan Lee, Byoung Hoon You, Sreymom Yim, Seung Yon Han, Hee-Sung Chae, Mingoo Bae, Seo-Yeon Kim, Jeong-Eun Yu, Jieun Jung, Piseth Nhoek, Hojun Kim, Han Seok Choi, Young-Won Chin, Hyun Woo Kim, Young Hee Choi
Frontiers in Pharmacology.2023;[Epub] CrossRef - A Comprehensive Review on Weight Loss Associated with Anti-Diabetic Medications
Fatma Haddad, Ghadeer Dokmak, Maryam Bader, Rafik Karaman
Life.2023; 13(4): 1012. CrossRef - The effects of acarbose treatment on cardiovascular risk factors in impaired glucose tolerance and diabetic patients: a systematic review and dose–response meta-analysis of randomized clinical trials
Mohammad Zamani, Mahlagha Nikbaf-Shandiz, Yasaman Aali, Niloufar Rasaei, Mahtab Zarei, Farideh Shiraseb, Omid Asbaghi
Frontiers in Nutrition.2023;[Epub] CrossRef - The effect of acarbose on lipid profiles in adults: a systematic review and meta-analysis of randomized clinical trials
Mohsen Yousefi, Sahand Tehrani Fateh, Mahlagha Nikbaf-Shandiz, Fatemeh Gholami, Samira Rastgoo, Reza Bagher, Alireza Khadem, Farideh Shiraseb, Omid Asbaghi
BMC Pharmacology and Toxicology.2023;[Epub] CrossRef - A systematic review, meta-analysis, dose-response, and meta-regression of the effects of acarbose intake on glycemic markers in adults
Sina Raissi Dehkordi, Naseh Pahlavani, Mahlagha Nikbaf-Shandiz, Reza Bagheri, Niloufar Rasaei, Melika Darzi, Samira Rastgoo, Hossein Bahari, Farideh Shiraseb, Omid Asbaghi
Journal of Diabetes & Metabolic Disorders.2023;[Epub] CrossRef - Inhibitory activity of xanthoangelol isolated from Ashitaba (Angelica keiskei Koidzumi) towards α-glucosidase and dipeptidyl peptidase-IV: in silico and in vitro studies
Diah Lia Aulifa, I Ketut Adnyana, Sukrasno Sukrasno, Jutti Levita
Heliyon.2022; 8(5): e09501. CrossRef - Design, synthesis, and in silico studies of benzimidazole bearing phenoxyacetamide derivatives as α-glucosidase and α-amylase inhibitors
Nahal Shayegan, Aida Iraji, Nasim Bakhshi, Ali Moazzam, Mohammad Ali Faramarzi, Somayeh Mojtabavi, Seyyed Mehrdad Mostafavi Pour, Maliheh Barazandeh Tehrani, Bagher Larijani, Zahra Rezaei, Pardis Yousefi, Mehdi Khoshneviszadeh, Mohammad Mahdavi
Journal of Molecular Structure.2022; 1268: 133650. CrossRef - American Association of Clinical Endocrinology Clinical Practice Guideline: Developing a Diabetes Mellitus Comprehensive Care Plan—2022 Update
Lawrence Blonde, Guillermo E. Umpierrez, S. Sethu Reddy, Janet B. McGill, Sarah L. Berga, Michael Bush, Suchitra Chandrasekaran, Ralph A. DeFronzo, Daniel Einhorn, Rodolfo J. Galindo, Thomas W. Gardner, Rajesh Garg, W. Timothy Garvey, Irl B. Hirsch, Danie
Endocrine Practice.2022; 28(10): 923. CrossRef - Combination of Bawang Dayak Extract and Acarbose against Male White Rat Glucose Levels
Aditya Maulana Perdana Putra, Ratih Pratiwi Sari, Siska Musiam
Borneo Journal of Pharmacy.2021; 4(2): 84. CrossRef - Natural α-Glucosidase and Protein Tyrosine Phosphatase 1B Inhibitors: A Source of Scaffold Molecules for Synthesis of New Multitarget Antidiabetic Drugs
Massimo Genovese, Ilaria Nesi, Anna Caselli, Paolo Paoli
Molecules.2021; 26(16): 4818. CrossRef - Impact of Simulated Gastrointestinal Conditions on Antiglycoxidant and α-Glucosidase Inhibition Capacities of Cyanidin-3-O-Glucoside
Didier Fraisse, Alexis Bred, Catherine Felgines, François Senejoux
Antioxidants.2021; 10(11): 1670. CrossRef
- The effect of acarbose on inflammatory cytokines and adipokines in adults: a systematic review and meta-analysis of randomized clinical trials
- Clinical Care/Education
- Reduction of Sulfonylurea with the Initiation of Basal Insulin in Patients with Inadequately Controlled Type 2 Diabetes Mellitus Undergoing Long-Term Sulfonylurea-Based Treatment
- Yeoree Yang, Jeong-Ah Shin, Hae Kyung Yang, Seung-Hwan Lee, Seung-Hyun Ko, Yu-Bae Ahn, Kun-Ho Yoon, Jae-Hyoung Cho
- Diabetes Metab J. 2016;40(6):454-462. Published online October 11, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.6.454
- 4,236 View
- 44 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background There were a limited number of studies about β-cell function after insulin initiation in patients exposed to long durations of sulfonylurea treatment. In this study, we aimed to evaluate the recovery of β-cell function and the efficacy of concurrent sulfonylurea use after the start of long-acting insulin.
Methods In this randomized controlled study, patients with type 2 diabetes mellitus (T2DM), receiving sulfonylurea for at least 2 years with glycosylated hemoglobin (HbA1c) >7%, were randomly assigned to two groups: sulfonylurea maintenance (SM) and sulfonylurea reduction (SR). Following a 75-g oral glucose tolerance test (OGTT), we administered long-acting basal insulin to the two groups. After a 6-month follow-up, we repeated the OGTT.
Results Among 69 enrolled patients, 57 completed the study and were analyzed: 31 in the SM and 26 in the SR group. At baseline, there was no significant difference except for the longer duration of diabetes and lower triglycerides in the SR group. After 6 months, the HbA1c was similarly reduced in both groups, but there was little difference in the insulin dose. In addition, insulin secretion during OGTT was significantly increased by 20% to 30% in both groups. A significant weight gain was observed in the SM group only. The insulinogenic index was more significantly improved in the SR group.
Conclusion Long-acting basal insulin replacement could improve the glycemic status and restore β-cell function in the T2DM patients undergoing sulfonylurea-based treatment, irrespective of the sulfonylurea dose reduction. The dose reduction of the concurrent sulfonylurea might be beneficial with regard to weight grain.
-
Citations
Citations to this article as recorded by- Initiating or Switching to Insulin Degludec/Insulin Aspart in Adults with Type 2 Diabetes: A Real-World, Prospective, Non-interventional Study Across Six Countries
Gregory R. Fulcher, Shahid Akhtar, Saleh J. Al-Jaser, Johan Medina, Mafauzy Mohamed, Nemencio A. Nicodemus, Anne Helene Olsen, Kiran P. Singh, Adri Kok
Advances in Therapy.2022; 39(8): 3735. CrossRef - Use of Insulin Glargine 100 U/mL for the Treatment of Type 2 Diabetes Mellitus in East Asians: A Review
Takahisa Hirose, Ching-Chu Chen, Kyu Jeung Ahn, Jacek Kiljański
Diabetes Therapy.2019; 10(3): 805. CrossRef - Insulin Therapy for Adult Patients with Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu-Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2017; 41(5): 367. CrossRef - Insulin therapy for adult patients with type 2 diabetes mellitus: a position statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
The Korean Journal of Internal Medicine.2017; 32(6): 967. CrossRef
- Initiating or Switching to Insulin Degludec/Insulin Aspart in Adults with Type 2 Diabetes: A Real-World, Prospective, Non-interventional Study Across Six Countries
- Complications
- Clinical Course and Risk Factors of Diabetic Retinopathy in Patients with Type 2 Diabetes Mellitus in Korea
- Jae-Seung Yun, Tae-Seok Lim, Seon-Ah Cha, Yu-Bae Ahn, Ki-Ho Song, Jin A Choi, Jinwoo Kwon, Donghyun Jee, Yang Kyung Cho, Yong-Moon Park, Seung-Hyun Ko
- Diabetes Metab J. 2016;40(6):482-493. Published online October 5, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.6.482
- 4,541 View
- 63 Download
- 30 Web of Science
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We investigated clinical course and risk factors for diabetic retinopathy (DR) in patients with type 2 diabetes mellitus (T2DM).
Methods A total of 759 patients with T2DM without DR were included from January 2001 to December 2004. Retinopathy evaluation was performed at least annually by ophthalmologists. The severity of the DR was classified into five categories according to the International Clinical Diabetic Retinopathy Severity Scales.
Results Of the 759 patients, 523 patients (68.9%) completed the follow-up evaluation. During the follow-up period, 235 patients (44.9%) developed DR, and 32 patients (13.6%) progressed to severe nonproliferative DR (NPDR) or proliferative DR (PDR). The mean duration of diabetes at the first diagnosis of mild NPDR, moderate NPDR, and severe NPDR or PDR were 14.8, 16.7, and 17.3 years, respectively. After adjusting multiple confounding factors, the significant risk factors for the incidence of DR risk in patients with T2DM were old age, longer duration of diabetes, higher mean glycosylated hemoglobin (HbA1c), and albuminuria. Even in the patients who had been diagnosed with diabetes for longer than 10 years at baseline, a decrease in HbA1c led to a significant reduction in the risk of developing DR (hazard ratio, 0.73 per 1% HbA1c decrement; 95% confidence interval, 0.58 to 0.91;
P =0.005).Conclusion This prospective cohort study demonstrates that glycemic control, diabetes duration, age, and albuminuria are important risk factors for the development of DR. More aggressive retinal screening for T2DM patients diagnosed with DR should be required in order to not miss rapid progression of DR.
-
Citations
Citations to this article as recorded by- Prevalence of diabetes and its correlates among Iranian adults: Results of the first phase of Shahedieh cohort study
Ali Dehghani, Hamid Korozhdehi, Saeid Hossein Khalilzadeh, Hossein Fallahzadeh, Vahid Rahmanian
Health Science Reports.2023;[Epub] CrossRef - Deep learning-based fundus image analysis for cardiovascular disease: a review
Symon Chikumba, Yuqian Hu, Jing Luo
Therapeutic Advances in Chronic Disease.2023;[Epub] CrossRef - Effect of anticoagulant/antiplatelet therapy on the development and progression of diabetic retinopathy
Chi-Juei Jeng, Yi-Ting Hsieh, Cheng-Li Lin, I-Jong Wang
BMC Ophthalmology.2022;[Epub] CrossRef - A deep learning model for screening type 2 diabetes from retinal photographs
Jae-Seung Yun, Jaesik Kim, Sang-Hyuk Jung, Seon-Ah Cha, Seung-Hyun Ko, Yu-Bae Ahn, Hong-Hee Won, Kyung-Ah Sohn, Dokyoon Kim
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(5): 1218. CrossRef - Risk factor analysis and clinical decision tree model construction for diabetic retinopathy in Western China
Yuan-Yuan Zhou, Tai-Cheng Zhou, Nan Chen, Guo-Zhong Zhou, Hong-Jian Zhou, Xing-Dong Li, Jin-Rui Wang, Chao-Fang Bai, Rong Long, Yu-Xin Xiong, Ying Yang
World Journal of Diabetes.2022; 13(11): 986. CrossRef - Association of Non-Alcoholic Fatty Liver Dis-ease and Diabetic Retinopathy in Patients with Type 2 Diabetes Mellitus: a Cross-Sectional Study
Zahra Heidari, Zahra Sharafi
Iranian South Medical Journal.2022; 25(1): 30. CrossRef - The Related Risk Factors of Diabetic Retinopathy in Elderly Patients with Type 2 Diabetes Mellitus: A Hospital-Based Cohort Study in Taiwan
Tsai-Tung Chiu, Tien-Lung Tsai, Mei-Yin Su, Tsan Yang, Peng-Lin Tseng, Yau-Jiunn Lee, Chao-Hsien Lee
International Journal of Environmental Research and Public Health.2021; 18(1): 307. CrossRef - Association of non‐alcoholic fatty liver disease with diabetic retinopathy in type 2 diabetic patients: A meta‐analysis of observational studies
Dandan Song, Chengqian Li, Zhongchao Wang, Yuhang Zhao, Baoming Shen, Wenjuan Zhao
Journal of Diabetes Investigation.2021; 12(8): 1471. CrossRef - PREVALENCE OF ADVANCED DIABETIC EYE DISEASE AND ITS ASSOCIATED RISK FACTORS IN TYPE 2 DIABETES MELLITUS
Likathung Ngullie, Bratatee Roy, Sayantan Ghosh, Sneha Jain, Lakshmi Kanta Mondal
INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH.2021; : 25. CrossRef - Progression of Diabetic Retinopathy and Declining Renal Function in Patients with Type 2 Diabetes
AJin Cho, Hayne Cho Park, Young-Ki Lee, Young Joo Shin, So Hyun Bae, Hakyoung Kim
Journal of Diabetes Research.2020; 2020: 1. CrossRef - First nation-wide study of diabetic retinopathy in Poland in the years 2013–2017
Milena Kozioł, Michał S. Nowak, Monika Udziela, Paweł Piątkiewicz, Iwona Grabska-Liberek, Jacek P. Szaflik
Acta Diabetologica.2020; 57(10): 1255. CrossRef - Awareness of diabetic retinopathy among Saudis with diabetes type 2 in Riyadh city
YousefM Alluhaymid, FawzanY Alotaibi, AbdulmajeedB Alotaibi, AbdullahM Albasha, AbdulrahmanS Alnaim, EssaM Sabi, AhmedH Mujamammi
Journal of Family Medicine and Primary Care.2020; 9(8): 4229. CrossRef - Relationship between Clinical Features of Diabetic Retinopathy and Systemic Factors in Patients with Newly Diagnosed Type II Diabetes Mellitus
Hyeseong Hwang, Jin Young Kim, Tae Keun Oh, Ju Byung Chae, Dong Yoon Kim
Journal of Korean Medical Science.2020;[Epub] CrossRef - Longitudinal Screening for Diabetic Retinopathy in a Nationwide Screening Program: Comparing Deep Learning and Human Graders
Jirawut Limwattanayingyong, Variya Nganthavee, Kasem Seresirikachorn, Tassapol Singalavanija, Ngamphol Soonthornworasiri, Varis Ruamviboonsuk, Chetan Rao, Rajiv Raman, Andrzej Grzybowski, Mike Schaekermann, Lily H. Peng, Dale R. Webster, Christopher Semtu
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Protective factors for diabetic retinopathy in Type 2 diabetes mellitus patients: Long duration of no less than 10 years
Yanli Liu, Chunwen Duan, Dejia Fang, Yi Liu, Hanchun Xu, Yarong Zheng, Yaling Xuan, Lili Wang, Lin Ye, Rui Su, Meixia An
Journal of Diabetes and its Complications.2019; 33(10): 107383. CrossRef - Incidence of sight‐threatening diabetic retinopathy in people with Type 2 diabetes mellitus and numbers needed to screen: a systematic review
Y. Groeneveld, D. Tavenier, J.W. Blom, B.C.P. Polak
Diabetic Medicine.2019; 36(10): 1199. CrossRef - Association between spousal diabetes status and diabetic retinopathy in Chinese patients with type 2 diabetes
Mei Yang, Yu Liu, Cuihong Wen, Beirui Wu, Xu Wan, Wei Luan, Jie Shen, Wei Liu, Jing Ma
Diabetes and Vascular Disease Research.2019; 16(5): 474. CrossRef - Presence of diabetic retinopathy is lower in type 2 diabetic patients with non-alcoholic fatty liver disease
Meng Zhang, Li Li, Jing Chen, Bei Li, Yutao Zhan, Chuan Zhang
Medicine.2019; 98(18): e15362. CrossRef - MicroRNAs as biomarkers of diabetic retinopathy and disease progression
Bridget Martinez, PhilipV Peplow
Neural Regeneration Research.2019; 14(11): 1858. CrossRef - Vascular changes in diabetic retinopathy—a longitudinal study in the Nile rat
Huishi Toh, Alexander Smolentsev, Rachel V. Bozadjian, Patrick W. Keeley, Madison D. Lockwood, Ryan Sadjadi, Dennis O. Clegg, Barbara A. Blodi, Peter J. Coffey, Benjamin E. Reese, James A. Thomson
Laboratory Investigation.2019; 99(10): 1547. CrossRef - DIABETE, TABAGISMO E DISASSUEFAZIONE DAL FUMO
Davide Campagna, Angela Alamo, Enrico Mondati, Riccardo Polosa
il Diabete.2019; 31(N. 1, marz): 41. CrossRef - Smoking and diabetes: dangerous liaisons and confusing relationships
D. Campagna, A. Alamo, A. Di Pino, C. Russo, A. E. Calogero, F. Purrello, R. Polosa
Diabetology & Metabolic Syndrome.2019;[Epub] CrossRef - Letter: Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study (Diabetes Metab J 2019;43:640–8)
Jun Sung Moon
Diabetes & Metabolism Journal.2019; 43(6): 911. CrossRef - Past and Current Status of Adult Type 2 Diabetes Mellitus Management in Korea: A National Health Insurance Service Database Analysis
Seung-Hyun Ko, Kyungdo Han, Yong-ho Lee, Junghyun Noh, Cheol-Young Park, Dae-Jung Kim, Chang Hee Jung, Ki-Up Lee, Kyung-Soo Ko
Diabetes & Metabolism Journal.2018; 42(2): 93. CrossRef - Excess visceral adiposity is associated with diabetic retinopathy in a multiethnic Asian cohort with longstanding type 2 diabetes
Angela Moh, Kumari Neelam, Xiao Zhang, Chee Fang Sum, Subramaniam Tavintharan, Keven Ang, Simon Biing Ming Lee, Wern Ee Tang, Su Chi Lim
Endocrine Research.2018; 43(3): 186. CrossRef - RNA sequencing identified specific circulating miRNA biomarkers for early detection of diabetes retinopathy
Zhen Liang, Kai P. Gao, Yi X. Wang, Zi C. Liu, Li Tian, Xin Z. Yang, Jing Y. Ding, Wei T. Wu, Wen H. Yang, Yi L. Li, Ze B. Zhang, Ri H. Zhai
American Journal of Physiology-Endocrinology and Metabolism.2018; 315(3): E374. CrossRef - High hemoglobin levels are associated with decreased risk of diabetic retinopathy in Korean type 2 diabetes
Min-Kyung Lee, Kyung-Do Han, Jae-Hyuk Lee, Seo-Young Sohn, Jee-Sun Jeong, Mee-Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Scientific Reports.2018;[Epub] CrossRef - Cigarette Smoking, Diabetes, and Diabetes Complications: Call for Urgent Action
Ping Zhu, Xiong-Fei Pan, Liting Sheng, Henggui Chen, An Pan
Current Diabetes Reports.2017;[Epub] CrossRef - Response: Features of Long-Standing Korean Type 2 Diabetes Mellitus Patients with Diabetic Retinopathy: A Study Based on Standardized Clinical Data (Diabetes Metab J 2017;41:393-404)
Sang Youl Rhee, Jeong-Taek Woo
Diabetes & Metabolism Journal.2017; 41(6): 494. CrossRef - Letter: Clinical Course and Risk Factors of Diabetic Retinopathy in Patients with Type 2 Diabetes Mellitus in Korea (Diabetes Metab J2016;40:482-93)
Nam Hoon Kim
Diabetes & Metabolism Journal.2017; 41(1): 75. CrossRef - Combined treatment of diabetic nephropathy with alprostadil and calcium dobesilate
Lili Qin, Wenjun Qin, Jianfei Wang, Lin Lin
Experimental and Therapeutic Medicine.2017;[Epub] CrossRef - Response: Clinical Course and Risk Factors of Diabetic Retinopathy in Patients with Type 2 Diabetes Mellitus in Korea (Diabetes Metab J2016;40:482-93)
Jae-Seung Yun, Seung-Hyun Ko
Diabetes & Metabolism Journal.2017; 41(1): 77. CrossRef - Clinical characteristics and risk factors for retinal diabetic neurodegeneration in type 2 diabetes
Kiyoung Kim, Eung Suk Kim, Sang Youl Rhee, Suk Chon, Jeong-taek Woo, Seung-Young Yu
Acta Diabetologica.2017; 54(11): 993. CrossRef - Letter: Features of Long-Standing Korean Type 2 Diabetes Mellitus Patients with Diabetic Retinopathy: A Study Based on Standardized Clinical Data (Diabetes Metab J 2017;41:393-404)
Jae-Seung Yun
Diabetes & Metabolism Journal.2017; 41(6): 492. CrossRef
- Prevalence of diabetes and its correlates among Iranian adults: Results of the first phase of Shahedieh cohort study
- Complications
- Baseline-Corrected QT (QTc) Interval Is Associated with Prolongation of QTc during Severe Hypoglycemia in Patients with Type 2 Diabetes Mellitus
- Seon-Ah Cha, Jae-Seung Yun, Tae-Seok Lim, Yoon-Goo Kang, Kang-Min Lee, Ki-Ho Song, Ki-Dong Yoo, Yong-Moon Park, Seung-Hyun Ko, Yu-Bae Ahn
- Diabetes Metab J. 2016;40(6):463-472. Published online October 5, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.6.463
- 3,680 View
- 47 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We investigated an association between baseline heart rate-corrected QT (QTc) interval before severe hypoglycemia (SH) and prolongation of QTc interval during SH in patients with type 2 diabetes mellitus (T2DM).
Methods Between January 2004 and June 2014, 208 patients with T2DM, who visited the emergency department because of SH and underwent standard 12-lead electrocardiography within the 6-month period before SH were consecutively enrolled. The QTc interval was analyzed during the incidence of SH, and 6 months before and after SH. QTc intervals of 450 ms or longer in men and 460 ms or longer in women were considered abnormally prolonged.
Results The mean age and diabetes duration were 68.1±12.1 and 14.1±10.1 years, respectively. The mean QTc intervals at baseline and SH episodes were 433±33 and 460±33 ms, respectively (
P <0.001). One hundred and fourteen patients (54.8%) had a prolonged QTc interval during SH. There was a significant decrease in the prolonged QTc interval within 6 months after SH (QTc interval prolongation during SH vs. after recovery, 54.8% vs. 33.8%,P <0.001). The prolonged QTc interval was significantly associated with baseline QTc interval prolongation (odds ratio, 2.92; 95% confidence interval, 1.22 to 6.96;P =0.016) after adjusting for multiple confounders.Conclusion A prolonged QTc interval at baseline was significantly associated with prolongation of the QTc interval during SH in patients with T2DM, suggesting the necessity of QTc interval monitoring and attention to those with a prolonged QTc interval to prevent SH.
-
Citations
Citations to this article as recorded by- Prevalence of QT prolongation and its risk factors in patients with type 2 diabetes
Khaled Aburisheh, Mohammad F. AlKheraiji, Saleh I. Alwalan, Arthur C. Isnani, Mohamed Rafiullah, Muhammad Mujammami, Assim A. Alfadda
BMC Endocrine Disorders.2023;[Epub] CrossRef - U-shaped association between the triglyceride–glucose index and atrial fibrillation incidence in a general population without known cardiovascular disease
Xiao Liu, Ayiguli Abudukeremu, Yuan Jiang, Zhengyu Cao, Maoxiong Wu, Jianyong Ma, Runlu Sun, Wanbing He, Zhiteng Chen, Yangxin Chen, Peng Yu, Wengen Zhu, Yuling Zhang, Jingfeng Wang
Cardiovascular Diabetology.2023;[Epub] CrossRef - Celebrities in the heart, strangers in the pancreatic beta cell: Voltage‐gated potassium channels Kv7.1 and Kv11.1 bridge long QT syndrome with hyperinsulinaemia as well as type 2 diabetes
Anniek F. Lubberding, Christian R. Juhl, Emil Z. Skovhøj, Jørgen K. Kanters, Thomas Mandrup‐Poulsen, Signe S. Torekov
Acta Physiologica.2022;[Epub] CrossRef - Severe hypoglycemia as a risk factor for cardiovascular outcomes in patients with type 2 diabetes: is it preventable?
Seung-Hyun Ko
Cardiovascular Prevention and Pharmacotherapy.2022; 4(3): 106. CrossRef - Heart rate-corrected QT interval prolongation is associated with decreased heart rate variability in patients with type 2 diabetes
Seon-Ah Cha
Medicine.2022; 101(45): e31511. CrossRef - Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus
Soo-Yeon Choi, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 263. CrossRef - Review of the cardiovascular safety of dipeptidyl peptidase-4 inhibitors and the clinical relevance of the CAROLINA trial
Marile Santamarina, Curt J. Carlson
BMC Cardiovascular Disorders.2019;[Epub] CrossRef - Antioxidant effects of epigallocatechin-3-gallate on the aTC1-6 pancreatic alpha cell line
Ting Cao, Xiong Zhang, Dan Yang, Yue-Qian Wang, Zheng-Dong Qiao, Jian-Ming Huang, Peng Zhang
Biochemical and Biophysical Research Communications.2018; 495(1): 693. CrossRef - Severe hypoglycemia is a risk factor for atrial fibrillation in type 2 diabetes mellitus: Nationwide population-based cohort study
Seung-Hyun Ko, Yong-Moon Park, Jae-Seung Yun, Seon-Ah Cha, Eue-Keun Choi, Kyungdo Han, Eugene Han, Yong-ho Lee, Yu-Bae Ahn
Journal of Diabetes and its Complications.2018; 32(2): 157. CrossRef - Incidence of prolonged QTc and severe hypoglycemia in type 1 diabetes: the EURODIAB Prospective Complications Study
Cristina Amione, Sara Giunti, Paolo Fornengo, Sabita S. Soedamah-Muthu, Nish Chaturvedi, J. H. Fuller, Federica Barutta, Gabriella Gruden, Graziella Bruno
Acta Diabetologica.2017; 54(9): 871. CrossRef
- Prevalence of QT prolongation and its risk factors in patients with type 2 diabetes
- Complications
- Severe Hypoglycemia and Cardiovascular or All-Cause Mortality in Patients with Type 2 Diabetes
- Seon-Ah Cha, Jae-Seung Yun, Tae-Seok Lim, Seawon Hwang, Eun-Jung Yim, Ki-Ho Song, Ki-Dong Yoo, Yong-Moon Park, Yu-Bae Ahn, Seung-Hyun Ko
- Diabetes Metab J. 2016;40(3):202-210. Published online April 5, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.202
- 4,465 View
- 60 Download
- 49 Web of Science
- 57 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We investigated the association between severe hypoglycemia (SH) and the risk of cardiovascular (CV) or all-cause mortality in patients with type 2 diabetes.
Methods The study included 1,260 patients aged 25 to 75 years with type 2 diabetes from the Vincent Type 2 Diabetes Resgistry (VDR), who consecutively enrolled (
n =1,260) from January 2000 to December 2010 and were followed up until May 2015 with a median follow-up time of 10.4 years. Primary outcomes were death from any cause or CV death. We investigated the association between the CV or all-cause mortality and various covariates using Cox proportional hazards regression analysis.Results Among the 906 participants (71.9%) who completed follow-up, 85 patients (9.4%) had at least one episode of SH, and 86 patients (9.5%) died (9.1 per 1,000 patient-years). Patients who had died were older, had a longer duration of diabetes and hypertension, received more insulin, and had more diabetic microvascular complications at baseline, as compared with surviving patients. The experience of SH was significantly associated with an increased risk of all-cause mortality (hazard ratio [HR], 2.64; 95% confidence interval [CI], 1.39 to 5.02;
P =0.003) and CV mortality (HR, 6.34; 95% CI, 2.02 to 19.87;P =0.002) after adjusting for sex, age, diabetic duration, hypertension, mean glycosylated hemoglobin levels, diabetic nephropathy, lipid profiles, and insulin use.Conclusion We found a strong association between SH and increased risk of all-cause and CV mortality in patients with type 2 diabetes.
-
Citations
Citations to this article as recorded by- The prognostic value of the stress hyperglycemia ratio for all-cause and cardiovascular mortality in patients with diabetes or prediabetes: insights from NHANES 2005–2018
Lei Ding, Hongda Zhang, Cong Dai, Aikai Zhang, Fengyuan Yu, Lijie Mi, Yingjie Qi, Min Tang
Cardiovascular Diabetology.2024;[Epub] CrossRef - Navigating the future of diabetes: innovative nomogram models for predicting all-cause mortality risk in diabetic nephropathy
Sensen Wu, Hui Wang, Dikang Pan, Julong Guo, Fan Zhang, Yachan Ning, Yongquan Gu, Lianrui Guo
BMC Nephrology.2024;[Epub] CrossRef - Association of hypoglycaemia with the risks of arrhythmia and mortality in individuals with diabetes - a systematic review and meta-analysis
Gangfeng Li, Shuping Zhong, Xingmu Wang, Fuyuan Zhuge
Frontiers in Endocrinology.2023;[Epub] CrossRef - Diabetes mellitus und Straßenverkehr – ein Positionspapier der Österreichischen Diabetesgesellschaft (Update 2023)
Heidemarie Abrahamian, Birgit Salamon, Angelika Lahnsteiner, Christian Schelkshorn, Alexander Bräuer, Lars Stechemesser, Gerd Köhler, Martin Clodi
Wiener klinische Wochenschrift.2023; 135(S1): 319. CrossRef - Validation of the hypoglycemia awareness questionnaire to assess hypoglycemia awareness in patients with type 2 diabetes treated with insulin
Diana Cristina Henao-Carrillo, Fabio Alexander Sierra-Matamoros, Ana Julia Carrillo Algarra, Julieth Patricia García-Lugo, Sandra Milena Hernández-Zambrano
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(12): 102917. CrossRef - Basal insulin analogues in people with diabetes and chronic kidney disease
David León‐Jiménez, José Pablo Miramontes‐González, Laura Márquez‐López, Francisco Astudillo‐Martín, Luis M. Beltrán‐Romero, Fernando Moreno‐Obregón, Javier Escalada‐San Martín
Diabetic Medicine.2022;[Epub] CrossRef - Severe Hypoglycemia Increases Dementia Risk and Related Mortality: A Nationwide, Population-based Cohort Study
Eugene Han, Kyung-do Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Seung-Hyun Ko, Yong-ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(5): e1976. CrossRef - Validación transcultural del HypoA-Q para medir conciencia de hipoglucemia en pacientes diabéticos
Ana Julia Carrillo-Algarra, Sandra Milena Hernandez-Zambrano, Fabio Alexander Sierra-Matamoros, Diana Cristina Henao-Carrillo, Ana María Gómez-Medina, Daniel Esteban Hurtado-Barrera
Revista Ciencia y Cuidado.2022; 19(1): 42. CrossRef - Validity of the diagnosis of diabetic microvascular complications in Korean national health insurance claim data
Hyung Jun Kim, Moo-Seok Park, Jee-Eun Kim, Tae-Jin Song
Annals of Clinical Neurophysiology.2022; 24(1): 7. CrossRef - Severe hypoglycemia as a risk factor for cardiovascular outcomes in patients with type 2 diabetes: is it preventable?
Seung-Hyun Ko
Cardiovascular Prevention and Pharmacotherapy.2022; 4(3): 106. CrossRef - Evaluation of a Clinical Platform to Promote Chronic Disease Management
Laura Greene, Nila Sathe, John A. House, Laura L. Schott, Stella Safo
Population Health Management.2021; 24(4): 470. CrossRef - Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus
Soo-Yeon Choi, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 263. CrossRef - Meta-Analysis: Association Between Hypoglycemia and Serious Adverse Events in Older Patients Treated With Glucose-Lowering Agents
Katharina Mattishent, Yoon K. Loke
Frontiers in Endocrinology.2021;[Epub] CrossRef - Epidemiology and outcomes from severe hypoglycemia in Kuwait: a prospective cohort study
Dalal Al Hasan, Ameen Yaseen, Mohammad Al Roudan, Lee Wallis
BMC Emergency Medicine.2021;[Epub] CrossRef - The incidence of hypoglycemia and its risk factors among diabetic patients in the Eastern Province of Saudi Arabia
Ahmed Elshebiny, Hassan Alali, Zainab Alamer, Yasmin Alsultan, Hashim Alkhalaf, Abdullah Alkishi, Mohammed Alsuwaylih
International Journal of Medicine in Developing Countries.2021; : 614. CrossRef - Current trends in epidemiology of cardiovascular disease and cardiovascular risk management in type 2 diabetes
Jae-Seung Yun, Seung-Hyun Ko
Metabolism.2021; 123: 154838. CrossRef - Real-world Evaluation of glycemic control and hypoglycemic Events among type 2 Diabetes mellitus study (REEDS): a multicentre, cross-sectional study in Thailand
Bancha Satirapoj, Thongchai Pratipanawatr, Boonsong Ongphiphadhanakul, Sompongse Suwanwalaikorn, Yupin Benjasuratwong, Wannee Nitiyanant
BMJ Open.2020; 10(2): e031612. CrossRef Predictors of Diabetes Self-Care Practice Among Patients with Type 2 Diabetes in Public Hospitals in Northeastern Ethiopia: A Facility-Based Cross-Sectional Study
Tesfaye Molla Gulentie, Ebrahim Mohammed Yesuf, Taklo Simeneh Yazie, Belayneh Kefale
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 3137. CrossRef- Hypoglycemia in Older Patients
Byron J. Hoogwerf
Clinics in Geriatric Medicine.2020; 36(3): 395. CrossRef - Severe hypoglycaemia and absolute risk of cause-specific mortality in individuals with type 2 diabetes: a UK primary care observational study
Francesco Zaccardi, Suping Ling, Claire Lawson, Melanie J. Davies, Kamlesh Khunti
Diabetologia.2020; 63(10): 2129. CrossRef - Insulin Glargine U100 Improved Glycemic Control and Reduced Nocturnal Hypoglycemia in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease Stages 3 and 4
Carolina C. Betônico, Silvia Maria O. Titan, Aécio Lira, Tatiana S. Pelaes, Maria Lúcia C. Correa-Giannella, Márcia Nery, Márcia Queiroz
Clinical Therapeutics.2019; 41(10): 2008. CrossRef - Efficacy and Safety of Degludec Compared to Glargine 300 Units/mL in Insulin-Experienced Patients With Type 2 Diabetes: Trial Protocol Amendment (NCT03078478)
Athena Philis-Tsimikas, Irene Stratton, Lone Nørgård Troelsen, Britta Anker Bak, Lawrence A. Leiter
Journal of Diabetes Science and Technology.2019; 13(3): 498. CrossRef - Efficacy and safety of insulin glargine/lixisenatide (iGlarLixi) fixed-ratio combination in older adults with type 2 diabetes
Yehuda Handelsman, Christina Chovanes, Terry Dex, Francesco Giorgino, Neil Skolnik, Elisabeth Souhami, William Stager, Elisabeth Niemoeller, Juan Pablo Frias
Journal of Diabetes and its Complications.2019; 33(3): 236. CrossRef - Urinary glucose excretion after dapagliflozin treatment: An exposure‐response modelling comparison between Japanese and non‐Japanese patients diagnosed with type 1 diabetes mellitus
Victor Sokolov, Tatiana Yakovleva, Shinya Ueda, Joanna Parkinson, David W. Boulton, Robert C. Penland, Weifeng Tang
Diabetes, Obesity and Metabolism.2019; 21(4): 829. CrossRef - Effects on clinical outcomes of intensifying triple oral antidiabetic drug (OAD) therapy by initiating insulin versus enhancing OAD therapy in patients with type 2 diabetes: A nationwide population‐based, propensity‐score‐matched cohort study
Shihchen Kuo, Chun‐Ting Yang, Jin‐Shang Wu, Huang‐Tz Ou
Diabetes, Obesity and Metabolism.2019; 21(2): 312. CrossRef - Cardiovascular safety and lower severe hypoglycaemia of insulin degludec versus insulin glargine U100 in patients with type 2 diabetes aged 65 years or older: Results from DEVOTE (DEVOTE 7)
Richard E. Pratley, Scott S. Emerson, Edward Franek, Matthew P. Gilbert, Steven P. Marso, Darren K. McGuire, Thomas R. Pieber, Bernard Zinman, Charlotte T. Hansen, Melissa V. Hansen, Thomas Mark, Alan C. Moses, John B. Buse
Diabetes, Obesity and Metabolism.2019; 21(7): 1625. CrossRef - Review of the cardiovascular safety of dipeptidyl peptidase-4 inhibitors and the clinical relevance of the CAROLINA trial
Marile Santamarina, Curt J. Carlson
BMC Cardiovascular Disorders.2019;[Epub] CrossRef - Effects of a 12-week moderate-intensity exercise training on blood glucose response in patients with type 2 diabetes
Shang-Lin Chiang, Margaret McLean Heitkemper, Yi-Jen Hung, Wen-Chii Tzeng, Meei-Shyuan Lee, Chia-Huei Lin
Medicine.2019; 98(36): e16860. CrossRef - Impaired Awareness of Hypoglycaemia in Insulin-treated Type 2 Diabetes Mellitus
Mohammad J. Alkhatatbeh, Nedaa A. Abdalqader , Mohammad A.Y. Alqudah
Current Diabetes Reviews.2019; 15(5): 407. CrossRef - Hypoglycaemia, cardiovascular disease, and mortality in diabetes: epidemiology, pathogenesis, and management
Stephanie A Amiel, Pablo Aschner, Belinda Childs, Philip E Cryer, Bastiaan E de Galan, Brian M Frier, Linda Gonder-Frederick, Simon R Heller, Timothy Jones, Kamlesh Khunti, Lawrence A Leiter, Yingying Luo, Rory J McCrimmon, Ulrik Pedersen-Bjergaard, Eliza
The Lancet Diabetes & Endocrinology.2019; 7(5): 385. CrossRef - Sulfonylureas as initial treatment for type 2 diabetes and the risk of adverse cardiovascular events: A population‐based cohort study
Kristian B. Filion, Antonios Douros, Laurent Azoulay, Hui Yin, Oriana H. Yu, Samy Suissa
British Journal of Clinical Pharmacology.2019; 85(10): 2378. CrossRef - Selectivity of beta-blockers, cardiovascular and all-cause mortality in people with hypoglycaemia: An observational study
F. Zaccardi, L.L. Nystrup Husemoen, B.L. Thorsted, D.R. Webb, S.K. Paul, M.J. Davies, K. Khunti
Nutrition, Metabolism and Cardiovascular Diseases.2019; 29(5): 481. CrossRef - Cost-effectiveness of a primary care multidisciplinary Risk Assessment and Management Program for patients with diabetes mellitus (RAMP-DM) over lifetime
Fangfang Jiao, Eric Yuk Fai Wan, Colman Siu Cheung Fung, Anca Ka Chun Chan, Sarah Morag McGhee, Ruby Lai Ping Kwok, Cindy Lo Kuen Lam
Endocrine.2019; 63(2): 259. CrossRef - Efficacy and safety of sensor-augmented pump therapy (SAPT) with predictive low-glucose management in patients diagnosed with type 1 diabetes mellitus previously treated with SAPT and low glucose suspend
Ana María Gómez, Diana Cristina Henao, Angelica Imitola, Oscar Mauricio Muñoz, Martín Alonso Rondón Sepúlveda, Laura Kattah, Juan Sebastian Guerrero, Elly Morros, Juan Pablo Llano, Maira García Jaramillo, Fabián León-Vargas
Endocrinología, Diabetes y Nutrición.2018; 65(8): 451. CrossRef - Recent diabetes-related mortality trends in Romania
Sorin Ioacara, Elisabeta Sava, Olivia Georgescu, Anca Sirbu, Simona Fica
Acta Diabetologica.2018; 55(8): 821. CrossRef - Use of sodium-glucose co-transporter-2 inhibitors from clinical trial results to practical application in Russia
D. A. Lebedev, A. Yu. Babenko
Medical Council.2018; (16): 100. CrossRef - Severe hypoglycemia is a risk factor for atrial fibrillation in type 2 diabetes mellitus: Nationwide population-based cohort study
Seung-Hyun Ko, Yong-Moon Park, Jae-Seung Yun, Seon-Ah Cha, Eue-Keun Choi, Kyungdo Han, Eugene Han, Yong-ho Lee, Yu-Bae Ahn
Journal of Diabetes and its Complications.2018; 32(2): 157. CrossRef - Antioxidant effects of epigallocatechin-3-gallate on the aTC1-6 pancreatic alpha cell line
Ting Cao, Xiong Zhang, Dan Yang, Yue-Qian Wang, Zheng-Dong Qiao, Jian-Ming Huang, Peng Zhang
Biochemical and Biophysical Research Communications.2018; 495(1): 693. CrossRef - Hemoglobin glycation index predicts cardiovascular disease in people with type 2 diabetes mellitus: A 10-year longitudinal cohort study
Mee Kyoung Kim, Jee Sun Jeong, Jae-Seung Yun, Hyuk-Sang Kwon, Ki Hyun Baek, Ki-Ho Song, Yu-Bae Ahn, Seung-Hyun Ko
Journal of Diabetes and its Complications.2018; 32(10): 906. CrossRef - Day-to-day fasting glycaemic variability in DEVOTE: associations with severe hypoglycaemia and cardiovascular outcomes (DEVOTE 2)
Bernard Zinman, Steven P. Marso, Neil R. Poulter, Scott S. Emerson, Thomas R. Pieber, Richard E. Pratley, Martin Lange, Kirstine Brown-Frandsen, Alan Moses, Ann Marie Ocampo Francisco, Jesper Barner Lekdorf, Kajsa Kvist, John B. Buse
Diabetologia.2018; 61(1): 48. CrossRef - Efficacy and safety of sensor-augmented pump therapy (SAPT) with predictive low-glucose management in patients diagnosed with type 1 diabetes mellitus previously treated with SAPT and low glucose suspend
Ana María Gómez, Diana Cristina Henao, Angelica Imitola, Oscar Mauricio Muñoz, Martín Alonso Rondón Sepúlveda, Laura Kattah, Juan Sebastian Guerrero, Elly Morros, Juan Pablo Llano, Maira García Jaramillo, Fabián León-Vargas
Endocrinología, Diabetes y Nutrición (English ed.).2018; 65(8): 451. CrossRef - Time- and frequency-domain measures of heart rate variability predict cardiovascular outcome in patients with type 2 diabetes
Seon-Ah Cha, Yong-Moon Park, Jae-Seung Yun, Seung-Hwan Lee, Yu-Bae Ahn, Sung-Rae Kim, Seung-Hyun Ko
Diabetes Research and Clinical Practice.2018; 143: 159. CrossRef - Newly diagnosed type 2 diabetes in an ethnic minority population: clinical presentation and comparison to other populations
Michael Morkos, Bettina Tahsin, Louis Fogg, Leon Fogelfeld
BMJ Open Diabetes Research & Care.2018; 6(1): e000568. CrossRef - DEVOTE 3: temporal relationships between severe hypoglycaemia, cardiovascular outcomes and mortality
Thomas R. Pieber, Steven P. Marso, Darren K. McGuire, Bernard Zinman, Neil R. Poulter, Scott S. Emerson, Richard E. Pratley, Vincent Woo, Simon Heller, Martin Lange, Kirstine Brown-Frandsen, Alan Moses, Jesper Barner Lekdorf, Lucine Lehmann, Kajsa Kvist,
Diabetologia.2018; 61(1): 58. CrossRef - Intervention effects of Compound Houttuyniae Herba to diabetic renal damage based on SOCS-JAK/STAT negative feedback regulation
Yun Fang, Sai-cong Shao, Hai-ying Wang
Chinese Herbal Medicines.2018; 10(4): 424. CrossRef - Monotherapy in Patients with Type 2 Diabetes Mellitus
Sang Youl Rhee, Hyun Jin Kim, Seung-Hyun Ko, Kyu-Yeon Hur, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 349. CrossRef - Monotherapy in patients with type 2 diabetes mellitus
Sang Youl Rhee, Hyun Jin Kim, Seung-Hyun Ko, Kyu Yeon Hur, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 959. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef - Cardiovascular effects of dipeptidyl peptidase-4 inhibitor in diabetic patients with and without established cardiovascular disease: a meta-analysis and systematic review
Shishi Xu, Xinyue Zhang, Lizhi Tang, Fang Zhang, Nanwei Tong
Postgraduate Medicine.2017; 129(2): 205. CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef - Effects of propofol on myocardial ischemia-reperfusion injury in rats with type-2 diabetes mellitus
Ying Wang, Xiuru Qi, Chunliang Wang, Danning Zhao, Hongjie Wang, Jianxin Zhang
Biomedical Reports.2017; 6(1): 69. CrossRef - Cardiovascular risk assessment in patients with diabetes
Marcello Casaccia Bertoluci, Viviane Zorzanelli Rocha
Diabetology & Metabolic Syndrome.2017;[Epub] CrossRef - Pathogenetic features of the combined course of arterial hypertension and diabetes mellitus 2 type
O.M. Bilovol, L.R. Bobronnikova, O.V. Al-Trawneh
Shidnoevropejskij zurnal vnutrisnoi ta simejnoi medicini.2017; 2017(1): 4. CrossRef - Risk Factors and Adverse Outcomes of Severe Hypoglycemia in Type 2 Diabetes Mellitus
Jae-Seung Yun, Seung-Hyun Ko
Diabetes & Metabolism Journal.2016; 40(6): 423. CrossRef - Real-world evidence for the safety of ipragliflozin in elderly Japanese patients with type 2 diabetes mellitus (STELLA-ELDER): final results of a post-marketing surveillance study
Koutaro Yokote, Yasuo Terauchi, Ichiro Nakamura, Haruko Sugamori
Expert Opinion on Pharmacotherapy.2016; 17(15): 1995. CrossRef - Hypoglycemia: Culprit or Bystander?
You-Cheol Hwang
Diabetes & Metabolism Journal.2016; 40(3): 190. CrossRef - Schwere Hypoglykämien erhöhen die Mortalität
E. Fritschka
MMW - Fortschritte der Medizin.2016; 158(S3): 46. CrossRef
- The prognostic value of the stress hyperglycemia ratio for all-cause and cardiovascular mortality in patients with diabetes or prediabetes: insights from NHANES 2005–2018
- Response: Cardiovascular Disease Predicts Severe Hypoglycemia in Patients with Type 2 Diabetes (
Diabetes Metab J 2015;39:498-506) - Jae-Seung Yun, Yu-Bae Ahn
- Diabetes Metab J. 2016;40(1):85-86. Published online February 19, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.1.85
- 2,750 View
- 29 Download
- Complications
- Cardiovascular Disease Predicts Severe Hypoglycemia in Patients with Type 2 Diabetes
- Jae-Seung Yun, Seung-Hyun Ko, Sun-Hye Ko, Ki-Ho Song, Ki-Dong Yoo, Kun-Ho Yoon, Yong-Moon Park, Yu-Bae Ahn
- Diabetes Metab J. 2015;39(6):498-506. Published online July 8, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.6.498
- 3,230 View
- 34 Download
- 20 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To investigate whether a history of prior cardiovascular disease (CVD) is associated with severe hypoglycemia (SH) in patients with type 2 diabetes.
Methods We conducted a prospective cohort study from January 2001 to December 2012 with a median follow-up time of 9.5 years (5,814 person-years). Patients aged 25 to 75 years with type 2 diabetes and without chronic kidney disease were enrolled (
n =894), and 624 patients completed follow-up. SH was defined as hypoglycemic episodes requiring hospitalization or medical care in an emergency department. We used the Cox proportional hazards regression analysis to test associations between SH episodes and potential explanatory variables.Results Among the 624 participants who completed follow-up, 60 patients (9.6%) had previous CVD. Compared to patients without CVD, patients with previous CVD were older, had a longer duration of diabetes and hypertension, received more insulin, and had more diabetic microvascular complications at baseline. During follow-up, 62 patients (9.9%) experienced at least one SH episode (incidence of 1.33 per 100 patient-years). The development of SH was associated with a history of CVD (hazard ratio, 1.99; 95% confidence interval, 1.07 to 3.72;
P =0.031) after adjusting for sex, age, diabetic duration, hypertension, hemoglobin A1c levels, diabetic complications, cardiovascular autonomic neuropathy, and insulin use.Conclusion A history of CVD was an independent risk factor for the development of SH in patients with type 2 diabetes mellitus. For patients with CVD, modulation of glycemic targets and diabetic education for the prevention of hypoglycemia should be implemented.
-
Citations
Citations to this article as recorded by- Evaluating the effectiveness of a novel somatostatin receptor 2 antagonist, ZT-01, for hypoglycemia prevention in a rodent model of type 2 diabetes
Ninoschka C. D’Souza, Julian A. Aiken, Emily G. Hoffman, Sara C. Atherley, Sabrina Champsi, Nadia Aleali, Dorsa Shakeri, Maya El-Zahed, Nicky Akbarian, Mehran Nejad-Mansouri, Parinaz Z. Bavani, Richard L. Liggins, Owen Chan, Michael C. Riddell
Frontiers in Pharmacology.2024;[Epub] CrossRef - Concomitant Use of Sulfonylureas and β-Blockers and the Risk of Severe Hypoglycemia Among Patients With Type 2 Diabetes: A Population-Based Cohort Study
Jenny Dimakos, Ying Cui, Robert W. Platt, Christel Renoux, Kristian B. Filion, Antonios Douros
Diabetes Care.2023; 46(2): 377. CrossRef - Evaluating the effect of Roxadustat on ventricular repolarization in patients undergoing peritoneal dialysis
Yangyang Zhang, Liang Zhang, Pengcheng Ge, Ruyi Xu, Zhen Ye
European Journal of Medical Research.2023;[Epub] CrossRef - Diabetic Neuropathy and Risk of Cardiovascular Disease
Jae-Seung Yun
The Journal of Korean Diabetes.2022; 23(4): 245. CrossRef - Randomised controlled trial of pharmacist-led patient counselling in controlling hypoglycaemic attacks in older adults with type 2 diabetes mellitus (ROSE-ADAM): A study protocol of the SUGAR intervention
Huda Y. Almomani, Carlos Rodriguez Pascual, Sayer I. Al-Azzam, Keivan Ahmadi
Research in Social and Administrative Pharmacy.2021; 17(5): 885. CrossRef - Diabetes and Frailty: An Expert Consensus Statement on the Management of Older Adults with Type 2 Diabetes
W. David Strain, Su Down, Pam Brown, Amar Puttanna, Alan Sinclair
Diabetes Therapy.2021; 12(5): 1227. CrossRef - Management of hypoglycemia in older adults with type 2 diabetes
Jeffrey Freeman
Postgraduate Medicine.2019; 131(4): 241. CrossRef - Use of stellate ganglion block for treatment of recurrent syncope followed by chest pain
Young-ung Kim, Yong-joon Shin, Young Woo Cho
Yeungnam University Journal of Medicine.2018; 35(1): 104. CrossRef - Coronary artery disease severity modifies associations between glycemic control and both mortality and myocardial infarction
Sridharan Raghavan, Wenhui G. Liu, P. Michael Ho, Mary E. Plomondon, Anna E. Barón, Liron Caplan, Karen E. Joynt Maddox, David Magid, David R. Saxon, Corrine I. Voils, Steven M. Bradley, Thomas M. Maddox
Journal of Diabetes and its Complications.2018; 32(5): 480. CrossRef - Depth and combined infection is important predictor of lower extremity amputations in hospitalized diabetic foot ulcer patients
Eun-Gyo Jeong, Sung Shim Cho, Sang-Hoon Lee, Kang-Min Lee, Seo-Kyung Woo, Yoongoo Kang, Jae-Seung Yun, Seon-Ah Cha, Yoon-Jung Kim, Yu-Bae Ahn, Seung-Hyun Ko, Jung-Min Lee
The Korean Journal of Internal Medicine.2018; 33(5): 952. CrossRef - Time- and frequency-domain measures of heart rate variability predict cardiovascular outcome in patients with type 2 diabetes
Seon-Ah Cha, Yong-Moon Park, Jae-Seung Yun, Seung-Hwan Lee, Yu-Bae Ahn, Sung-Rae Kim, Seung-Hyun Ko
Diabetes Research and Clinical Practice.2018; 143: 159. CrossRef - Risk Factors for Severe Hypoglycemia in Black and White Adults With Diabetes: The Atherosclerosis Risk in Communities (ARIC) Study
Alexandra K. Lee, Clare J. Lee, Elbert S. Huang, A. Richey Sharrett, Josef Coresh, Elizabeth Selvin
Diabetes Care.2017; 40(12): 1661. CrossRef - Early inner retinal thinning and cardiovascular autonomic dysfunction in type 2 diabetes
Jin A. Choi, Hyo Won Kim, Jin-Woo Kwon, Yun-sub Shim, Dong Hyun Jee, Jae-Seung Yun, Yu-Bae Ahn, Chan Kee Park, Seung-Hyun Ko, Patrice E. Fort
PLOS ONE.2017; 12(3): e0174377. CrossRef - Cardiovascular Autonomic Dysfunction Predicts Diabetic Foot Ulcers in Patients With Type 2 Diabetes Without Diabetic Polyneuropathy
Jae-Seung Yun, Seon-Ah Cha, Tae-Seok Lim, Eun-Young Lee, Ki-Ho Song, Yu-Bae Ahn, Ki-Dong Yoo, Joon-Sung Kim, Yong-Moon Park, Seung-Hyun Ko
Medicine.2016; 95(12): e3128. CrossRef - Clinical Course and Risk Factors of Diabetic Retinopathy in Patients with Type 2 Diabetes Mellitus in Korea
Jae-Seung Yun, Tae-Seok Lim, Seon-Ah Cha, Yu-Bae Ahn, Ki-Ho Song, Jin A Choi, Jinwoo Kwon, Donghyun Jee, Yang Kyung Cho, Yong-Moon Park, Seung-Hyun Ko
Diabetes & Metabolism Journal.2016; 40(6): 482. CrossRef - Diabetic Cardiovascular Autonomic Neuropathy Predicts Recurrent Cardiovascular Diseases in Patients with Type 2 Diabetes
Seon-Ah Cha, Jae-Seung Yun, Tae-Seok Lim, Kyoungil Min, Ki-Ho Song, Ki-Dong Yoo, Yong-Moon Park, Yu-Bae Ahn, Seung-Hyun Ko, James M Wright
PLOS ONE.2016; 11(10): e0164807. CrossRef - Meta-analysis: Association between hypoglycaemia and serious adverse events in older patients
Katharina Mattishent, Yoon Kong Loke
Journal of Diabetes and its Complications.2016; 30(5): 811. CrossRef - Letter: Cardiovascular Disease Predicts Severe Hypoglycemia in Patients with Type 2 Diabetes (Diabetes Metab J 2015;39:498-506)
Mi-Kyung Kim
Diabetes & Metabolism Journal.2016; 40(1): 83. CrossRef - Response: Cardiovascular Disease Predicts Severe Hypoglycemia in Patients with Type 2 Diabetes (Diabetes Metab J 2015;39:498-506)
Jae-Seung Yun, Yu-Bae Ahn
Diabetes & Metabolism Journal.2016; 40(1): 85. CrossRef - Lipoprotein(a) predicts a new onset of chronic kidney disease in people with Type 2 diabetes mellitus
J.‐S. Yun, Y.‐B. Ahn, K.‐H. Song, K.‐D. Yoo, Y.‐M. Park, H.‐W. Kim, S.‐H. Ko
Diabetic Medicine.2016; 33(5): 639. CrossRef - Severe Hypoglycemia and Cardiovascular Disease in Type 2 Diabetes
Hyeong Kyu Park
Diabetes & Metabolism Journal.2015; 39(6): 478. CrossRef
- Evaluating the effectiveness of a novel somatostatin receptor 2 antagonist, ZT-01, for hypoglycemia prevention in a rodent model of type 2 diabetes
- Intensive Individualized Reinforcement Education Is Important for the Prevention of Hypoglycemia in Patients with Type 2 Diabetes
- Yun-Mi Yong, Kyung-Mi Shin, Kang-Min Lee, Jae-Young Cho, Sun-Hye Ko, Min-Hyang Yoon, Tae-Won Kim, Jong-Hyun Jeong, Yong-Moon Park, Seung-Hyun Ko, Yu-Bae Ahn
- Diabetes Metab J. 2015;39(2):154-163. Published online March 10, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.2.154
- 3,952 View
- 40 Download
- 17 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We investigated whether an intensive individualized reinforcement education program could influence the prevention of hypoglycemic events in patients with type 2 diabetes.
Methods From March 2013 to September 2013, patients aged 35 to 75 years with type 2 diabetes who had not previously participated in diabetes education, and treated with insulin or a sulfonylurea-containing regimen were included in the study. After structured group education, the patients assigned to the intensive individualized education group (IT) were requested to visit for reinforcement. All subjects in the IT were encouraged to self-manage dose adjustments. Participants in both groups (control group [CG, group education only;
n =22] and IT [n =24]) attended follow-up visits at 2, 8, 12, and 24 weeks. At each visit, all patients were asked whether they had experienced hypoglycemia.Results The total study population consisted of 20 men (43.5%; mean age and diabetic duration of 55.9±11.0 and 5.1±7.3 years, respectively). At 24 weeks, there were no significant differences in hemoglobin A1c values between the CG and IT. The total number of hypoglycemic events per patient was 5.26±6.5 in the CG and 2.58±2.3 times in the IT (
P =0.004). Adherence to lifestyle modification including frequency of exercise, self-monitoring of blood glucose, or dietary habit was not significantly different between the groups. However, adherence to hypoglycemia management, especially the dose adjustment of medication, was significantly higher in the IT compared with the CG.Conclusion Compared with the structured group education, additional IT resulted in additional benefits in terms of avoidance of hypoglycemia and treating hypoglycemia in patients with type 2 diabetes.
-
Citations
Citations to this article as recorded by- Effectiveness of the SUGAR intervention on hypoglycaemia in elderly patients with type 2 diabetes: A pragmatic randomised controlled trial
Huda Y. Almomani, Carlos Rodriguez Pascual, Paul Grassby, Keivan Ahmadi
Research in Social and Administrative Pharmacy.2023; 19(2): 322. CrossRef - A Cross-Sectional study on risk factors for severe hypoglycemia among Insulin-Treated elderly type 2 diabetes Mellitus (T2DM) patients in Singapore
Michelle Shi Min Ko, Wai Kit Lee, Li Chang Ang, Su-Yen Goh, Yong Mong Bee, Ming Ming Teh
Diabetes Research and Clinical Practice.2022; 185: 109236. CrossRef - Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study
Jin Hee Jung, Jung Hwa Lee, Hyang Mi Jang, Young Na, Hee Sun Choi, Yeon Hee Lee, Yang Gyo Kang, Na Rae Kim, Jeong Rim Lee, Bok Rye Song, Kang Hee Sim
The Journal of Korean Diabetes.2022; 23(1): 64. CrossRef - Anti-hyperglycemic Medication Compliance: A Quality Assurance Project
Rayan Mamoon, Md Y Mamoon, Debbie Hermanstyne, Issac Sachmechi
Cureus.2022;[Epub] CrossRef - Randomised controlled trial of pharmacist-led patient counselling in controlling hypoglycaemic attacks in older adults with type 2 diabetes mellitus (ROSE-ADAM): A study protocol of the SUGAR intervention
Huda Y. Almomani, Carlos Rodriguez Pascual, Sayer I. Al-Azzam, Keivan Ahmadi
Research in Social and Administrative Pharmacy.2021; 17(5): 885. CrossRef - Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus
Soo-Yeon Choi, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 263. CrossRef - Type 2 diabetes patients’ views on prevention of hypoglycaemia – a mixed methods study investigating self-management issues and self-identified causes of hypoglycaemia
Stijn Crutzen, Tessa van den Born-Bondt, Petra Denig, Katja Taxis
BMC Family Practice.2021;[Epub] CrossRef - Cross‐sectional analysis of emergency hypoglycaemia and outcome predictors among people with diabetes in an urban population
Chukwuma Uduku, Valentina Pendolino, Ian Godsland, Nick Oliver, Monika Reddy, Rachael T. Fothergill
Diabetic Medicine.2021;[Epub] CrossRef - Short-term efficacy of high intensity group and individual education in patients with type 2 diabetes: a randomized single-center trial
R. Reale, A. Tumminia, L. Romeo, N. La Spina, R. Baratta, G. Padova, L. Tomaselli, L. Frittitta
Journal of Endocrinological Investigation.2019; 42(4): 403. CrossRef - The role of structured education in the management of hypoglycaemia
Ahmed Iqbal, Simon R. Heller
Diabetologia.2018; 61(4): 751. CrossRef - Association of diabetes therapy-related quality of life and physical activity levels in patients with type 2 diabetes receiving medication therapy: the Diabetes Distress and Care Registry at Tenri (DDCRT 17)
Yasuaki Hayashino, Satoru Tsujii, Hitoshi Ishii
Acta Diabetologica.2018; 55(2): 165. CrossRef - Insulin Therapy for Adult Patients with Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu-Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2017; 41(5): 367. CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef - Insulin therapy for adult patients with type 2 diabetes mellitus: a position statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
The Korean Journal of Internal Medicine.2017; 32(6): 967. CrossRef - Physician-Directed Diabetes Education without a Medication Change and Associated Patient Outcomes
Hun-Sung Kim, Hyunah Kim, Hae-Kyung Yang, Eun Young Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung-Hwan Lee, Jae Hyoung Cho, In Young Choi, Hyeon Woo Yim, Bong-Yun Cha
Diabetes & Metabolism Journal.2017; 41(3): 187. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef - Hypoglycemia and Health Costs
Yong-ho Lee, Gyuri Kim, Eun Seok Kang
The Journal of Korean Diabetes.2016; 17(1): 11. CrossRef - Association between estimated blood glucose levels and glycated hemoglobin levels
Seon-Ah Cha, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2016; 31(3): 457. CrossRef - Characteristics of Hypoglycemia Pateints Visiting the Emergency Department of a University Hospital
Sang-Hyeon Choi, Deok-Ki Youn, Moon-Gi Choi, Ohk-Hyun Ryu
The Journal of Korean Diabetes.2016; 17(3): 202. CrossRef - Experiences of Diabetes Education among Educators of Diabetes : a content analysis approach
Soo Jin Kang, Soo Jung Chang
Journal of Korean Public Health Nursing.2016; 30(2): 221. CrossRef
- Effectiveness of the SUGAR intervention on hypoglycaemia in elderly patients with type 2 diabetes: A pragmatic randomised controlled trial
- Statin Discontinuation after Achieving a Target Low Density Lipoprotein Cholesterol Level in Type 2 Diabetic Patients without Cardiovascular Disease: A Randomized Controlled Study
- Seung-Hwan Lee, Hyuk-Sang Kwon, Yong-Moon Park, Seung-Hyun Ko, Yoon-Hee Choi, Kun-Ho Yoon, Yu-Bae Ahn
- Diabetes Metab J. 2014;38(1):64-73. Published online February 19, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.1.64
- 3,881 View
- 48 Download
- 16 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background This study investigated the rate of relapse of dyslipidemia and the factors which could predict relapse following a short-term statin discontinuation after achieving a target low density lipoprotein cholesterol (LDL-C) level in type 2 diabetic patients without cardiovascular disease (CVD).
Methods Ninety-nine subjects on rosuvastatin treatment and whose LDL-C level was lower than 100 mg/dL were randomly assigned to discontinue or maintain statin treatment at a 2:1 ratio. The subjects were followed-up after 10 weeks. A relapse of dyslipidemia was defined as a reascent of LDL-C level to greater than 100 mg/dL.
Results The statin discontinuation group had a significant rate of relapse compared to the maintenance group (79% vs. 3%, respectively). Pretreatment and baseline lipid levels, their ratios, and hemoglobin A1c level were significantly different between the relapse and nonrelapse groups. The pretreatment and baseline lipid profiles and their ratios were independently associated with relapse. The pretreatment LDL-C level was the most useful parameter for predicting a relapse, with a cutoff of 123 mg/dL. During the follow-up period, no CVD event was noted.
Conclusion The relapse rate of dyslipidemia was high when statins were discontinued in type 2 diabetic patients without CVD. Statin discontinuation should be considered carefully based on the pretreatment lipid profiles of patients.
-
Citations
Citations to this article as recorded by- Cardiovascular Outcomes and Mortality Associated With Discontinuing Statins in Older Patients Receiving Polypharmacy
Federico Rea, Annalisa Biffi, Raffaella Ronco, Matteo Franchi, Simona Cammarota, Anna Citarella, Valeria Conti, Amelia Filippelli, Carmine Sellitto, Giovanni Corrao
JAMA Network Open.2021; 4(6): e2113186. CrossRef - Visit-to-visit variability of lipid measurements and the risk of myocardial infarction and all-cause mortality: A prospective cohort study
Xiaoxue Liu, Shouling Wu, Qiaofeng Song, Xizhu Wang
Atherosclerosis.2020; 312: 110. CrossRef - 2018 Guidelines for the management of dyslipidemia
Eun-Jung Rhee, Hyeon Chang Kim, Jae Hyeon Kim, Eun Young Lee, Byung Jin Kim, Eun Mi Kim, YoonJu Song, Jeong Hyun Lim, Hae Jin Kim, Seonghoon Choi, Min Kyong Moon, Jin Oh Na, Kwang-Yeol Park, Mi Sun Oh, Sang Youb Han, Junghyun Noh, Kyung Hee Yi, Sang-Hak L
The Korean Journal of Internal Medicine.2019; 34(4): 723. CrossRef - 2018 Guidelines for the Management of Dyslipidemia in Korea
Eun-Jung Rhee, Hyeon Chang Kim, Jae Hyeon Kim, Eun Young Lee, Byung Jin Kim, Eun Mi Kim, YoonJu Song, Jeong Hyun Lim, Hae Jin Kim, Seonghoon Choi, Min Kyong Moon, Jin Oh Na, Kwang-Yeol Park, Mi Sun Oh, Sang Youb Han, Junghyun Noh, Kyung Hee Yi, Sang-Hak L
Journal of Lipid and Atherosclerosis.2019; 8(2): 78. CrossRef - Patterns of statin use and long‐term adherence and persistence among older adults with diabetes
Richard Ofori‐Asenso, Jenni Ilomäki, Mark Tacey, Ella Zomer, Andrea J. Curtis, J. Simon Bell, Sophia Zoungas, Danny Liew
Journal of Diabetes.2018; 10(9): 699. CrossRef - Effect of visit-to-visit LDL-, HDL-, and non-HDL-cholesterol variability on mortality and cardiovascular outcomes after percutaneous coronary intervention
Eun Young Lee, Yeoree Yang, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Wook Sung Chung, Seung-Hwan Lee, Kiyuk Chang
Atherosclerosis.2018; 279: 1. CrossRef - Change in ALT levels after administration of HMG‐CoA reductase inhibitors to subjects with pretreatment levels three times the upper normal limit in clinical practice
Hyunah Kim, Hyeseon Lee, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung‐Hwan Lee, Jae‐Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun‐Ho Yoon, Hun‐Sung Kim
Cardiovascular Therapeutics.2018;[Epub] CrossRef - Orthodox religious fasting as a medical nutrition therapy for dyslipidemia: where do we stand and how far can we go?
Theocharis Koufakis, Spyridon N Karras, Pantelis Zebekakis, Kalliopi Kotsa
European Journal of Clinical Nutrition.2018; 72(4): 474. CrossRef - Phenotyping of Korean patients with better-than-expected efficacy of moderate-intensity statins using tensor factorization
Jingyun Choi, Yejin Kim, Hun-Sung Kim, In Young Choi, Hwanjo Yu, Katriina Aalto-Setala
PLOS ONE.2018; 13(6): e0197518. CrossRef - Impact of educational outreach intervention on enhancing health care providers' knowledge about statin therapy prescribing in Malaysian patients with type 2 diabetes mellitus
Mohamed Hassan Elnaem, Mohamad Haniki Nik Mohamed, Hasniza Zaman Huri, Shah M Azarisman
Journal of Evaluation in Clinical Practice.2018; 24(3): 521. CrossRef - Use of Moderate‐Intensity Statins for Low‐Density Lipoprotein Cholesterol Level above 190 mg/dL at Baseline in Koreans
Hun‐Sung Kim, Hyeseon Lee, Sue Hyun Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Sun Jung Baik, Hyunah Kim, Seung‐Hwan Lee, Jae Hyoung Cho, In‐Young Choi, Kun‐Ho Yoon, Ju Han Kim
Basic & Clinical Pharmacology & Toxicology.2017; 121(4): 272. CrossRef - Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
European Heart Journal.2017; 38(48): 3560. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - The differences in the incidence of diabetes mellitus and prediabetes according to the type of HMG-CoA reductase inhibitors prescribed in Korean patients
Tong Min Kim, Hyunah Kim, Yoo Jin Jeong, Sun Jung Baik, So Jung Yang, Seung-Hwan Lee, Jae-Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun-Ho Yoon, Hun-Sung Kim
Pharmacoepidemiology and Drug Safety.2017; 26(10): 1156. CrossRef - Statin for the Primary Prevention of Cardiovascular Disease in Patients with Diabetes Mellitus
Bo Kyung Koo
Diabetes & Metabolism Journal.2014; 38(1): 32. CrossRef
- Cardiovascular Outcomes and Mortality Associated With Discontinuing Statins in Older Patients Receiving Polypharmacy
- Erratum: Author's Name Correction. Diabetic Retinopathy and Endothelial Dysfunction in Patients with Type 2 Diabetes Mellitus
- Jae-Seung Yun, Seung-Hyun Ko, Ji-Hoon Kim, Keon-Woong Moon, Yong-Moon Park, Ki-Dong Yoo, Yu-Bae Ahn
- Diabetes Metab J. 2013;37(6):488-488. Published online December 12, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.6.488
- 2,695 View
- 23 Download
- 1 Crossref
- Response: Diabetic Retinopathy and Endothelial Dysfunction in Patients with Type 2 Diabetes Mellitus (
Diabetes Metab J 2013;37:262-9) - Jae-Seung Yun, Yu-Bae Ahn
- Diabetes Metab J. 2013;37(5):393-394. Published online October 17, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.5.393
- 2,439 View
- 24 Download
- 1 Crossref
-
 PDF
PDF PubReader
PubReader -
Citations
Citations to this article as recorded by- Effect of ascorbic acid, α-tocopherol and its combination on human umbilical vein endothelial cells permeability exposed to high concentration of glucose
Yudi Purnomo, Djoko W. Soeatmadji, M. Aris Widodo
Russian Open Medical Journal.2020;[Epub] CrossRef
- Effect of ascorbic acid, α-tocopherol and its combination on human umbilical vein endothelial cells permeability exposed to high concentration of glucose
- Diabetic Retinopathy and Endothelial Dysfunction in Patients with Type 2 Diabetes Mellitus
- Jae-Seung Yun, Seung-Hyun Ko, Ji-Hoon Kim, Kun-Woong Moon, Yong-Moon Park, Ki-Dong Yoo, Yu-Bae Ahn
- Diabetes Metab J. 2013;37(4):262-269. Published online August 14, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.4.262
- 3,911 View
- 33 Download
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We investigated the relationship between endothelial dysfunction and diabetic retinopathy (DR) in patients with type 2 diabetes.
Methods We used a cross-sectional design to examine 167 patients with type 2 diabetes mellitus. All patients underwent biochemical and ophthalmological examination. We assessed endothelial dysfunction by a flow-mediated vasodilation method of the brachial artery. Changes in vasodilation (flow-mediated vasodilatation, %FMD) were expressed as percent change over baseline values.
Results The mean±standard deviation of patient age was 54.1±8.6 years. The %FMD was significantly lower in patients with DR than without DR. The prevalence of retinopathy decreased across increasing tertiles of %FMD. After adjusting for patients' age, sex, diabetes duration, use of insulin, use of antihypertensive, antiplatelet, and lipid lowering medications, systolic blood pressure, fasting plasma glucose, 2-hour plasma glucose, glycated hemoglobin, and urinary albumin excretion, participants with a reduced %FMD were more likely to have DR (odds ratio, 11.819; 95% confidence interval, 2.201 to 63.461;
P =0.004, comparing the lowest and highest tertiles of %FMD).Conclusion Endothelial dysfunction was associated with DR, which was most apparent when the endothelial dysfunction was severe. Our study provides insights into the possible mechanism of the influence of endothelial dysfunction on the development of DR.
-
Citations
Citations to this article as recorded by- Effects of Methylenetetrahydrofolate Reductase (MTHFR) Polymorphisms on Retinal Tissue Perfusion in Mild Diabetic Retinopathy Patients Receiving the Medical Food, Ocufolin®
Hong Jiang, Zhiping Liu, Justin H Townsend, Jianhua Wang
Clinical Ophthalmology.2023; Volume 17: 1121. CrossRef - Cardiometabolic risk factors, peripheral arterial tonometry and metformin in adults with type 1 diabetes participating in the REducing with MetfOrmin Vascular Adverse Lesions trial
David Chen, Alicia J Jenkins, Nicola Greenlaw, Katie Dudman, Tamsin Fernandes, David M Carty, Alun D Hughes, Andrzej S Januszewski, Coen DA Stehouwer, John R Petrie
Diabetes and Vascular Disease Research.2023;[Epub] CrossRef - Micro (mi) RNA and Diabetic Retinopathy
Sadashiv, Praveen Sharma, Shailendra Dwivedi, Sunita Tiwari, Pankaj Kumar Singh, Amit Pal, Sandeep Kumar
Indian Journal of Clinical Biochemistry.2022; 37(3): 267. CrossRef - Ethnomedicinal Value of Antidiabetic Plants in Bangladesh: A Comprehensive Review
Md. Masudur Rahman, Md. Josim Uddin, A. S. M. Ali Reza, Abu Montakim Tareq, Talha Bin Emran, Jesus Simal-Gandara
Plants.2021; 10(4): 729. CrossRef - Relating Retinal Vascular Oxygen Saturation and Microvasculature Morphology at Progressive Stages of Diabetic Retinopathy
Selin L. Auvazian, Jennifer Cano, Sophie Leahy, Preny Karamian, Amir Kashani, Andrew Moshfeghi, Hossein Ameri, Norman P. Blair, Mahnaz Shahidi
Translational Vision Science & Technology.2021; 10(6): 4. CrossRef - Renalase gene Glu37Asp polymorphism affects susceptibility to diabetic retinopathy in type 2 diabetes mellitus
Monika Buraczynska, Karolina Gwiazda-Tyndel, Bartłomiej Drop, Wojciech Zaluska
Acta Diabetologica.2021; 58(12): 1595. CrossRef - Endothelium as a Therapeutic Target in Diabetes Mellitus: From Basic Mechanisms to Clinical Practice
Anastasios Tentolouris, Ioanna Eleftheriadou, Evangelia Tzeravini, Dimitrios Tsilingiris, Stavroula A. Paschou, Gerasimos Siasos, Nikolaos Tentolouris
Current Medicinal Chemistry.2020; 27(7): 1089. CrossRef - miR‐181a/b‐5p regulates human umbilical vein endothelial cell angiogenesis by targeting PDGFRA
Tingting Sun, Linan Yin, Hongyu Kuang
Cell Biochemistry and Function.2020; 38(2): 222. CrossRef - The role of microRNAs in the healing of diabetic ulcers
Golnaz Goodarzi, Mahmood Maniati, Durdi Qujeq
International Wound Journal.2019; 16(3): 621. CrossRef - Role of altered coagulation-fibrinolytic system in the pathophysiology of diabetic retinopathy
Tapan Behl, Thirumurthy Velpandian, Anita Kotwani
Vascular Pharmacology.2017; 92: 1. CrossRef - Macular oedema as manifestation of diabetic retinopathy
Mukharram M. Bikbov, Rinat R. Fayzrakhmanov, Rinat M. Zaynullin, Artur F. Zaynetdinov, Timur R. Gilmanshin, Marat R. Kalanov
Diabetes mellitus.2017; 20(4): 263. CrossRef - Shedding light on miR-26a: Another key regulator of angiogenesis in diabetic wound healing
Carlos Zgheib, Kenneth W. Liechty
Journal of Molecular and Cellular Cardiology.2016; 92: 203. CrossRef - Lipoprotein(a) predicts the development of diabetic retinopathy in people with type 2 diabetes mellitus
Jae-Seung Yun, Tae-Seok Lim, Seon-Ah Cha, Yu-Bae Ahn, Ki-Ho Song, Jin A. Choi, Jinwoo Kwon, Donghyun Jee, Yang Kyung Cho, Yong-Moon Park, Seung-Hyun Ko
Journal of Clinical Lipidology.2016; 10(2): 426. CrossRef - Clinical Course and Risk Factors of Diabetic Retinopathy in Patients with Type 2 Diabetes Mellitus in Korea
Jae-Seung Yun, Tae-Seok Lim, Seon-Ah Cha, Yu-Bae Ahn, Ki-Ho Song, Jin A Choi, Jinwoo Kwon, Donghyun Jee, Yang Kyung Cho, Yong-Moon Park, Seung-Hyun Ko
Diabetes & Metabolism Journal.2016; 40(6): 482. CrossRef - Relationship of systemic endothelial function and peripheral arterial stiffness with diabetic retinopathy
Laurence S Lim, Lieng H Ling, Chui Ming Gemmy Cheung, Peng Guan Ong, Lingli Gong, E Shyong Tai, Ranjana Mathur, Doric Wong, Wallace Foulds, Tien Yin Wong
British Journal of Ophthalmology.2015; 99(6): 837. CrossRef - Retinal Nerve Fiber Layer Loss Is Associated with Urinary Albumin Excretion in Patients with Type 2 Diabetes
Jin A. Choi, Sun-Hee Ko, Yi Ryeung Park, Dong-Hyun Jee, Seung-Hyun Ko, Chan Kee Park
Ophthalmology.2015; 122(5): 976. CrossRef - Flow Mediated Dilatation Is Reduced with the Progressive Stages of Glomerular Filtration Rate and Albuminuria in Type 2 Diabetic Patients without Coronary Heart Disease
Hiroyuki Ito, Mina Nakashima, Kentaro Meguro, Haruki Furukawa, Hitomi Yamashita, Akifusa Takaki, Chizuko Yukawa, Takashi Omoto, Masahiro Shinozaki, Shinya Nishio, Mariko Abe, Shinichi Antoku, Mizuo Mifune, Michiko Togane
Journal of Diabetes Research.2015; 2015: 1. CrossRef - The Role of MicroRNAs in Diabetic Complications—Special Emphasis on Wound Healing
João Moura, Elisabet Børsheim, Eugenia Carvalho
Genes.2014; 5(4): 926. CrossRef - Role of AMP‐Activated Protein Kinase in Cancer Therapy
Gauhar Rehman, Adeeb Shehzad, Abdul Latif Khan, Muhammad Hamayun
Archiv der Pharmazie.2014; 347(7): 457. CrossRef - Urinary albumin excretion rate: a risk factor for retinal hard exudates in macular region in type 2 diabetic patients
Shaocheng Wang, Siyong Lin, Xi Cao, Yuezhong Zheng, Jinyang Wang, Na Lu, Jinkui Yang
Chinese Medical Journal.2014; 127(12): 2293. CrossRef - Letter: Diabetic Retinopathy and Endothelial Dysfunction in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2013;37:262-9)
Seok Man Son
Diabetes & Metabolism Journal.2013; 37(5): 391. CrossRef
- Effects of Methylenetetrahydrofolate Reductase (MTHFR) Polymorphisms on Retinal Tissue Perfusion in Mild Diabetic Retinopathy Patients Receiving the Medical Food, Ocufolin®
- Influence of the Duration of Diabetes on the Outcome of a Diabetes Self-Management Education Program
- Seung-Hyun Ko, Sin-Ae Park, Jae-Hyoung Cho, Sun-Hye Ko, Kyung-Mi Shin, Seung-Hwan Lee, Ki-Ho Song, Yong-Moon Park, Yu-Bae Ahn
- Diabetes Metab J. 2012;36(3):222-229. Published online June 14, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.3.222
- 4,215 View
- 41 Download
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Diabetes education and lifestyle modification are critical components in controlling blood glucose levels of people with type 2 diabetes. Until now, available data on the effectiveness of education with respect to the duration of diabetes are limited. We investigated whether adherence to lifestyle behavior modification prompted by diabetes education was influenced by the duration of diabetes.
Methods Two hundred and twenty-five people with type 2 diabetes were recruited for an intensive, collaborative, group-based diabetes education program with annual reinforcement. We divided the patients into two groups based on the duration of their diabetes prior to the education program (≤1 year [≤1Y] vs. ≥3 years [≥3Y]). Dietary habits, physical activity, and the frequency of blood glucose self-monitoring were evaluated with a questionnaire prior to education and at the follow-up endpoint.
Results The mean follow-up period was 32.2 months. The mean hemoglobin A1c (A1C) value was significantly lower in the ≤1Y group. Self-care behaviors, measured by scores for dietary habits (
P =0.004) and physical activity (P <0.001), were higher at the endpoint in the ≤1Y group than in the ≥3Y group. Logistic regression analysis revealed that a longer diabetes duration before education was significantly associated with mean A1C levels greater than or equal to 7.0% (53 mmol/mol).Conclusion Diabetes duration influenced the effectiveness of diabetes education on lifestyle behavior modification and glycemic control. More-intense, regular, and sustained reinforcement with encouragement may be required for individuals with longstanding type 2 diabetes.
-
Citations
Citations to this article as recorded by- Prevalence of type 2 diabetes complications and its association with diet knowledge and skills and self‐care barriers in Tabriz, Iran: A cross‐sectional study
Habib Jalilian, Elnaz Javanshir, Leila Torkzadeh, Saeedeh Fehresti, Nazanin Mir, Majid Heidari‐Jamebozorgi, Somayeh Heydari
Health Science Reports.2023;[Epub] CrossRef - Continuing the quality improvement of an electronic personal health record and interactive website for people with diabetes in Scotland (My Diabetes My Way)
Cathy Shields, Nicholas T. Conway, Brian Allardice, Deborah J. Wake, Scott G. Cunningham
Diabetic Medicine.2023;[Epub] CrossRef - The use of nomogram for detecting mild cognitive impairment in patients with type 2 diabetes mellitus
Rehanguli Maimaitituerxun, Wenhang Chen, Jingsha Xiang, Yu Xie, Atipatsa C. Kaminga, Xin Yin Wu, Letao Chen, Jianzhou Yang, Aizhong Liu, Wenjie Dai
Journal of Diabetes.2023; 15(5): 448. CrossRef - DENTAL IMPLANT TREATMENT IN DIABETES MELLITUS (DM) PATIENTS: REVIEW
Hakob Khachatryan
BULLETIN OF STOMATOLOGY AND MAXILLOFACIAL SURGERY.2023; : 121. CrossRef - An association between socioeconomic status and preventive screening for diabetic eye and kidney complications among individuals with type 2 diabetes
Changwoo Shon, Jongnam Hwang
Korean Journal of Health Education and Promotion.2023; 40(5): 27. CrossRef - Association of quality of life with medication adherence and glycemic control in patients with type 1 diabetes
Farimah Fayyaz, Parham Mardi, Sahar Sobhani, Leily Sokoty, Fatemeh Aghamahdi, Mostafa Qorbani
Journal of Diabetes & Metabolic Disorders.2023;[Epub] CrossRef - Effect of aerobic training on baroreflex sensitivity, heart rate recovery, and heart rate variability in type 2 diabetes: a systematic review
Sarah Parveen, Muhammad Azharuddin, Majumi M. Noohu
International Journal of Diabetes in Developing Countries.2023;[Epub] CrossRef - Managing type 2 diabetes and depression with Mindfulness-integrated Cognitive Behavior Therapy (MiCBT)
Fateh Sohrabi, Ahmad Sohrabi, Narges Shams-Alizadeh, Bruno A. Cayoun
Discover Psychology.2022;[Epub] CrossRef - Perception of benefits and barriers associated with dementia prevention behaviors among people with diabetes
Noppamas Pipatpiboon, Nut Koonrungsesomboon, Wachira Suriyawong, Jirapas Sripetchwandee, Sue Turale
Nursing & Health Sciences.2022; 24(1): 274. CrossRef - An exploratory study on the knowledge, attitude and practice of sharp disposal among type 2 diabetes mellitus patients in Northern Peninsular Malaysia
Jin Yi Choo, Yen Ping Ng, Ahmad Kamal Ariffin Abdul Jamil, Wei Kai Heng, Yee Mei Ng, Jing Ng, Cheng Hoon Yap
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(4): 102479. CrossRef - Efficacy of Personalized Diabetes Self-care Using an Electronic Medical Record–Integrated Mobile App in Patients With Type 2 Diabetes: 6-Month Randomized Controlled Trial
Eun Young Lee, Seon-Ah Cha, Jae-Seung Yun, Sun-Young Lim, Jin-Hee Lee, Yu-Bae Ahn, Kun-Ho Yoon, Min Kyung Hyun, Seung-Hyun Ko
Journal of Medical Internet Research.2022; 24(7): e37430. CrossRef - Real-world Benefits of Diabetes Management App Use and Self-monitoring of Blood Glucose on Glycemic Control: Retrospective Analyses
Ya-Ting Chang, Yu-Zhen Tu, Hung-Yi Chiou, Ken Lai, Neng Chun Yu
JMIR mHealth and uHealth.2022; 10(6): e31764. CrossRef - Glycemic control and its influencing factors in type 2 diabetes patients in Anhui, China
Xiu-Ya Xing, Xin-Yi Wang, Xi Fang, Jing-Qiao Xu, Ye-Ji Chen, Wei Xu, Hua-Dong Wang, Zhi-Rong Liu, Sha-Sha Tao
Frontiers in Public Health.2022;[Epub] CrossRef - Time for Using Machine Learning for Dose Guidance in Titration of People With Type 2 Diabetes? A Systematic Review of Basal Insulin Dose Guidance
Camilla Heisel Nyholm Thomsen, Stine Hangaard, Thomas Kronborg, Peter Vestergaard, Ole Hejlesen, Morten Hasselstrøm Jensen
Journal of Diabetes Science and Technology.2022; : 193229682211459. CrossRef - Adherence to Mediterranean diet and advanced glycation endproducts in patients with diabetes
Marko Grahovac, Marko Kumric, Marino Vilovic, Dinko Martinovic, Ante Kreso, Tina Ticinovic Kurir, Josip Vrdoljak, Karlo Prizmic, Joško Božić
World Journal of Diabetes.2021; 12(11): 1942. CrossRef - Impact of Diabetes and Disease Duration on Work Status Among U.S. Older Adults
Miriam Mutambudzi, Cesar Gonzalez Gonzalez, Rebecca Wong
Journal of Aging and Health.2020; 32(5-6): 432. CrossRef - The association of illness perceptions and God locus of health control with self-care behaviours in patients with type 2 diabetes in Saudi Arabia
Mohsen Alyami, Anna Serlachius, Ibrahim Mokhtar, Elizabeth Broadbent
Health Psychology and Behavioral Medicine.2020; 8(1): 329. CrossRef - The Impact of a Community-Based Food Education Program on Nutrition-Related Knowledge in Middle-Aged and Older Patients with Type 2 Diabetes: Results of a Pilot Randomized Controlled Trial
Carlos Vasconcelos, António Almeida, Maria Cabral, Elisabete Ramos, Romeu Mendes
International Journal of Environmental Research and Public Health.2019; 16(13): 2403. CrossRef - Diabetes-Related Health Care Utilization and Dietary Intake Among Food Pantry Clients
Eric M. Bomberg, Sophie Rosenmoss, Morgan Smith, Elaine Waxman, Hilary K. Seligman
Health Equity.2019; 3(1): 644. CrossRef - Factors Contributing to Sharp Waste Disposal at Health Care Facility Among Diabetic Patients in North-East Peninsular Malaysia
Ummu Atiyyah Hasan, Suhaily Mohd Hairon, Najib Majdi Yaacob, Aziah Daud, Anees Abdul Hamid, Norzaihan Hassan, Mohd Faiz Ariffin, Lau Yi Vun
International Journal of Environmental Research and Public Health.2019; 16(13): 2251. CrossRef - Effectiveness of Diabetes Community Sharp Disposal Education Module in Primary Care: An Experimental Study in North-East Peninsular Malaysia
Ummu Atiyyah Hasan, Suhaily Mohd Hairon, Najib Majdi Yaacob, Aziah Daud, Anees Abdul Hamid, Norzaihan Hassan, Mohd Faiz Ariffin, Lau Yi Vun
International Journal of Environmental Research and Public Health.2019; 16(18): 3356. CrossRef - Analysis of the Relationship between the Referral and Evolution of Patients with Type 2 Diabetes Mellitus
Camilo Alvarez, Cecilia Saint-Pierre, Valeria Herskovic, Marcos Sepúlveda
International Journal of Environmental Research and Public Health.2018; 15(7): 1534. CrossRef - Clinical characteristics of Chinese patients with duration of type 2 diabetes >40 years
Tingting Song, Yingying Luo, Xuhui Wang, Jing Li, Qian Han, Hong Zhu, Wei Zhao, Weidong Li, Zhong Sun, Xilin Yang
Journal of Diabetes.2017; 9(1): 45. CrossRef - Impacto de intervenções educativas na redução das complicações diabéticas: revisão sistemática
Marcela Machado Menezes, Camila Takáo Lopes, Lilia de Souza Nogueira
Revista Brasileira de Enfermagem.2016; 69(4): 773. CrossRef - The Well-Being and Treatment Satisfaction of Diabetic Patients in an Outpatient Setting at a General Hospital in Korea
Hwa-Sun Park, Sin Na Lee, Min Young Baek, Seung Hee Yu, Young Sil Eom, Sihoon Lee, Ki Young Lee, Yeun Sun Kim, Byung Joon Kim, Kwang Won Kim, Ie Byung Park
The Journal of Korean Diabetes.2016; 17(2): 123. CrossRef - Poor glycemic control in type 2 diabetes in the South of the Sahara: The issue of limited access to an HbA1c test
Alioune Camara, Naby M. Baldé, Joelle Sobngwi-Tambekou, André P. Kengne, Mansour M. Diallo, Alain P.K. Tchatchoua, Amadou Kaké, Ngamani Sylvie, Beverley Balkau, Fabrice Bonnet, Eugène Sobngwi
Diabetes Research and Clinical Practice.2015; 108(1): 187. CrossRef - Effect of Group Training on Glycemic Control in Patients With Diabetes Type-I
Marjan Naseri, Shahnaz Rostami, Bahman Dashtebozorgi
Jundishapur Journal of Chronic Disease Care.2015;[Epub] CrossRef - Clinical audit of patients using DPP4 inhibitors in longstanding type 2 diabetes
K.V.S. Hari Kumar, A.K. Gupta
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2015; 9(4): 277. CrossRef - Moderate diet-induced weight loss is associated with improved insulin sensitivity in middle-aged healthy obese Korean women
Hye-Ok Lee, Jung-Eun Yim, Young-Seol Kim, Ryowon Choue
Nutrition Research and Practice.2014; 8(4): 469. CrossRef - Inverse Association between Glycated Albumin and Insulin Secretory Function May Explain Higher Levels of Glycated Albumin in Subjects with Longer Duration of Diabetes
Yong-ho Lee, Mi Hyang Kown, Kwang Joon Kim, Eun Young Lee, Daham Kim, Byung-Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee, Marià Alemany
PLoS ONE.2014; 9(9): e108772. CrossRef - Systematic review of the psychometric properties and theoretical grounding of instruments evaluating self‐care in people with type 2 Diabetes Mellitus
Jorge Caro‐Bautista, Francisco Javier Martín‐Santos, Jose Miguel Morales‐Asencio
Journal of Advanced Nursing.2014; 70(6): 1209. CrossRef - It's Still Not Too Late to Make a Change: Current Status of Glycemic Control in Korea
Sang Yong Kim
Diabetes & Metabolism Journal.2014; 38(3): 194. CrossRef - Efficacy of the Smartphone-Based Glucose Management Application Stratified by User Satisfaction
Hun-Sung Kim, Wona Choi, Eun Kyoung Baek, Yun A Kim, So Jung Yang, In Young Choi, Kun-Ho Yoon, Jae-Hyoung Cho
Diabetes & Metabolism Journal.2014; 38(3): 204. CrossRef - Education as Prescription for Patients with Type 2 Diabetes Mellitus: Compliance and Efficacy in Clinical Practice
Mi Yeon Kim, Sunghwan Suh, Sang-Man Jin, Se Won Kim, Ji Cheol Bae, Kyu Yeon Hur, Sung Hye Kim, Mi Yong Rha, Young Yun Cho, Myung-Shik Lee, Moon Kyu Lee, Kwang-Won Kim, Jae Hyeon Kim
Diabetes & Metabolism Journal.2012; 36(6): 452. CrossRef
- Prevalence of type 2 diabetes complications and its association with diet knowledge and skills and self‐care barriers in Tabriz, Iran: A cross‐sectional study

 KDA
KDA
 First
First Prev
Prev





